Case Studies in Ophthalmology
Cases for the Ophthalmology Clerkship
Note to Medical Students on the Ophthalmology Rotation at the University of Iowa:
Print the question and answer sheet (Ctrl-Print or Command-Print) and enter your answers on it. You may prefer to type your answers on this page and then print it. If you do this, be careful that your full answer shows in the printout. Experience with Internet Explorer has been less than optimal.
Return the printed copy with your answers to Michelle Snyder or Dr. Kemp via campus mail (11290 PFP) or scan as a pdf and email to Michelle at michelle-r-snyder@uiowa.edu or Dr. Kemp at pavlina-kemp@uiowa.edu.
Case #6 Third Nerve Palsy
History
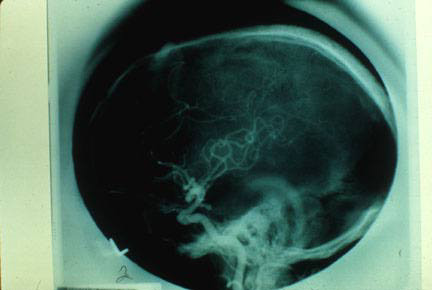
58- year-old woman with lifelong history of migraine develops a severe headache different from her usual migraines. 36 hours into the headache she develops an incomplete third nerve palsy with a dilated pupil.
Photo #1
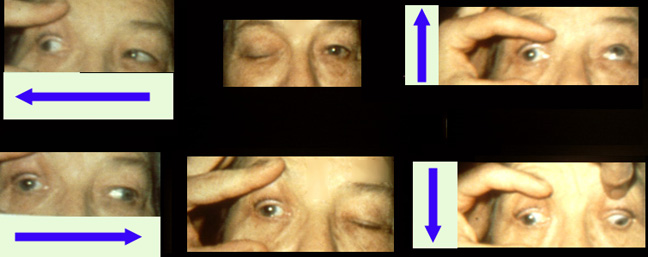
Photo #2
Enter Full Name (required):
Your email address (required):
Question #1
What historical questions would you like answered?
Question #2
What tests would you order and in what sequence?
Question #3
Is this an emergency? Why or why not?
Question #4
What is the significance of the large pupil?
Question #5
Would you expect this person to develop aberrant regeneration of her third nerve?
Question #6
What are the classic pathophysiologic mechanisms of third nerve palsy?
Question #7
What anatomical location of the third nerve is involved in this case?
Question #8
What age range is ophthalmoplegic migraine ususally seen?
References
Green W, Hackett E, Schlezinger N: Neuro-ophthalmologic evaluation of oculomotor nerve paralysis. Arch Ophthalmol 1964; 72:154.
Rush JA, Younge BR: Paralysis of cranial nerves III, IV, V. Cause and prognosis in 1000 cases. Arch Ophthalmol. 1981; 99:76.
Schatz JA, Savino PJ, Corbett JJ: Primary aberrant oculomotor regeneration. A sign of cavernous meningioma. Arch Neurol. 1977; 34:29.
Corbett JJ: Neuro-ophthalmic complications of migraine and cluster headaches. Neurol Clin. 1983; 1: 973-995.