
This patient is a 78-year-old man with known history of high-risk non-exudative age-related macular degeneration, and full-thickness macular hole in the left eye, presented for annual follow-up. He noted rapid decline in vision in his formerly better-seeing right eye since three months prior to presentation. No pain or irritation. He has no history of prior intravitreal injections. No other complaints.
BCVA cc:
IOP: OD 15, OS 14
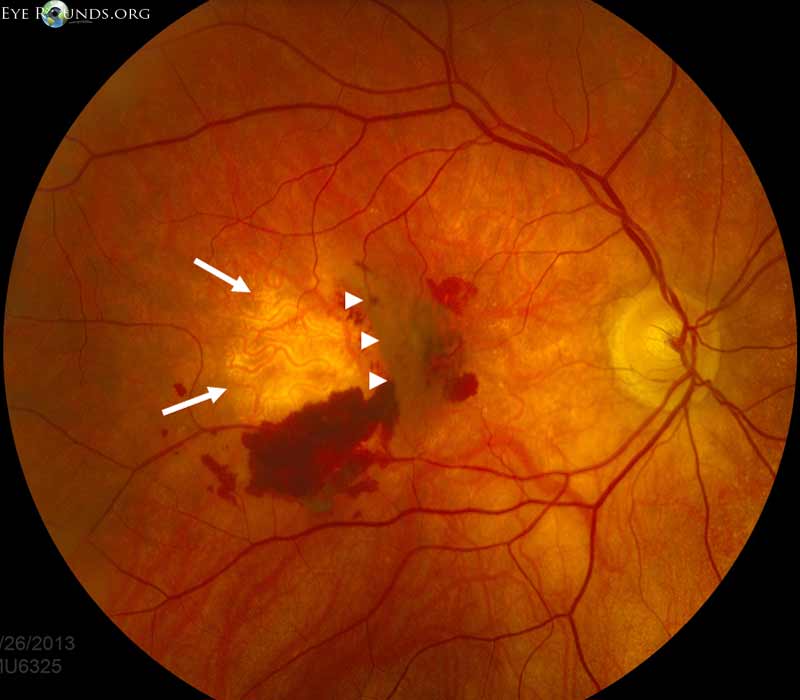


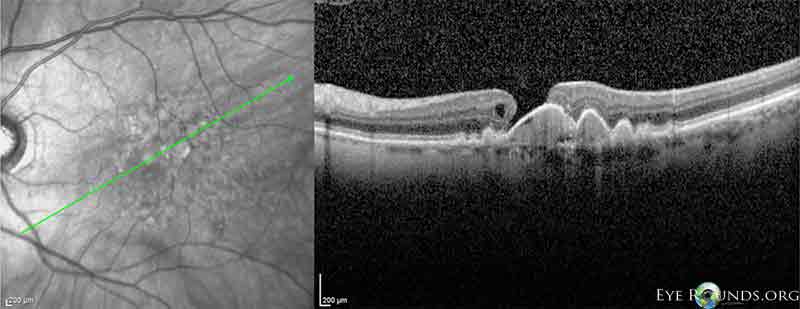
RPE detachments have known to develop RPE rips, either spontaneously or following laser photocoagulation, photodynamic therapy, or intravitreal injection. They usually occur at or along the edge of the serous RPE detachment.
Mechanisms include fibrovascular contraction of choroidal neovascular membranes, mechanical forces from vitreomacular traction or interruption of tight junctions due to anti-VEGF therapy.
An incidence of 10% has been reported as part of the natural history of macular degeneration.
Improvement in visual acuity may occur after treatment (usually anti-VEGF or photodynamic therapy) despite RPE rips, but the patient and clinician need to be aware of this situation, as it may warrant close follow-up and re-treatment in cases of deterioration.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.