
Retinopathy associated with leukemia typically occurs in acute disease.
Patients may develop dilation, tortuosity, and beading of the retinal veins; vascular sheathing; cotton-wool spots; flame-shaped hemorrhages; Roth spots; sub-hyaloid and sub-internal limiting membrane hemorrhages. These changes are similar to those seen with severe anemia.
A 60-year-old female was referred for bilateral retinal hemorrhages. She noticed blurry since two months prior when she hit her head. She said her right eye gradually improved, but the left eye remained poor. She was told that this may be related to her blood pressure, but it was found to be normal (i.e. 118/70). She had a past ocular history of myopia, and a past medical history of hypertension.
BCVA with correction:
IOP: OD 13; OS 14
SLE: anterior segment unremarkable; 1+ NS OU; no AC cells; no vitreous cells
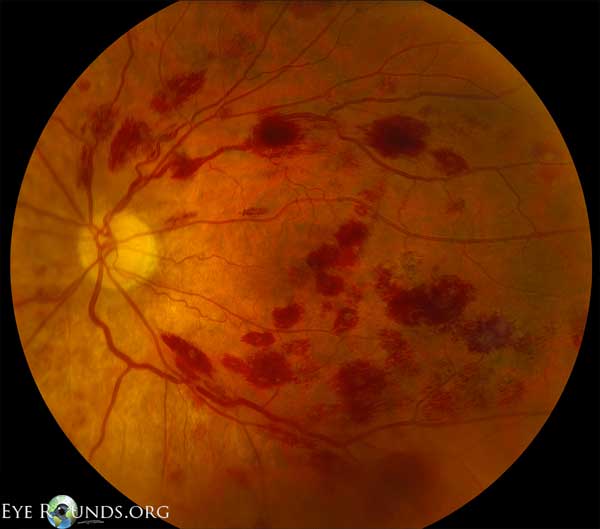
The patient presented with bilateral retinal hemorrhages and scattered Roth spots. A fluorescein angiogram was done which ruled out retinal venous occlusions and showed no evidence of vasculitis.
Upon further history, she reported mild fatigue and bruising on the upper and lower extremities for the past few weeks.
CBC, ESR, CRP, ANA were ordered, significant for the following:
Patient was immediately referred to the hematology and oncology service. She was diagnosed with leukocytosis consistent with chronic myeloid leukemia, later found to be positive for the Philadelphia (Ph+) chromosome.
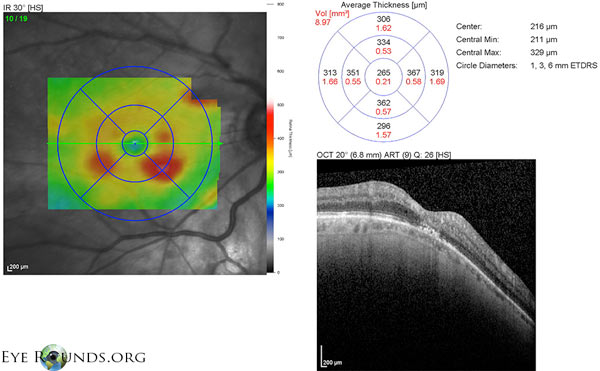
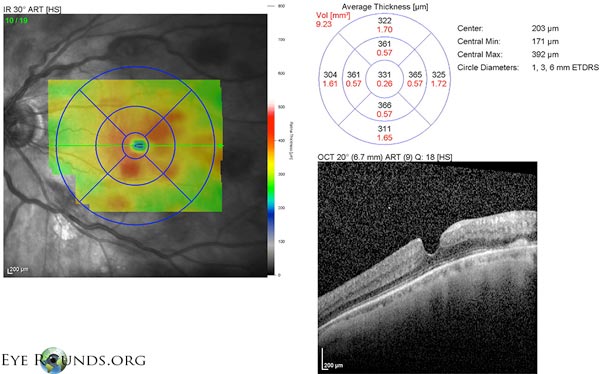
She was started on chemotherapy, and her follow-up fundus photos are shown below.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.