
A 20-year-old male was referred by an optometrist because of a pigmented scar in the right eye. The patient complained of black spots in his vision for the past week. He had no pain or irritation. He was born in Peru, but came to the United States at the age of 14 and lived in Tennessee on a farm and had been exposed to many cats in the past. He had no other complaints or medical problems.


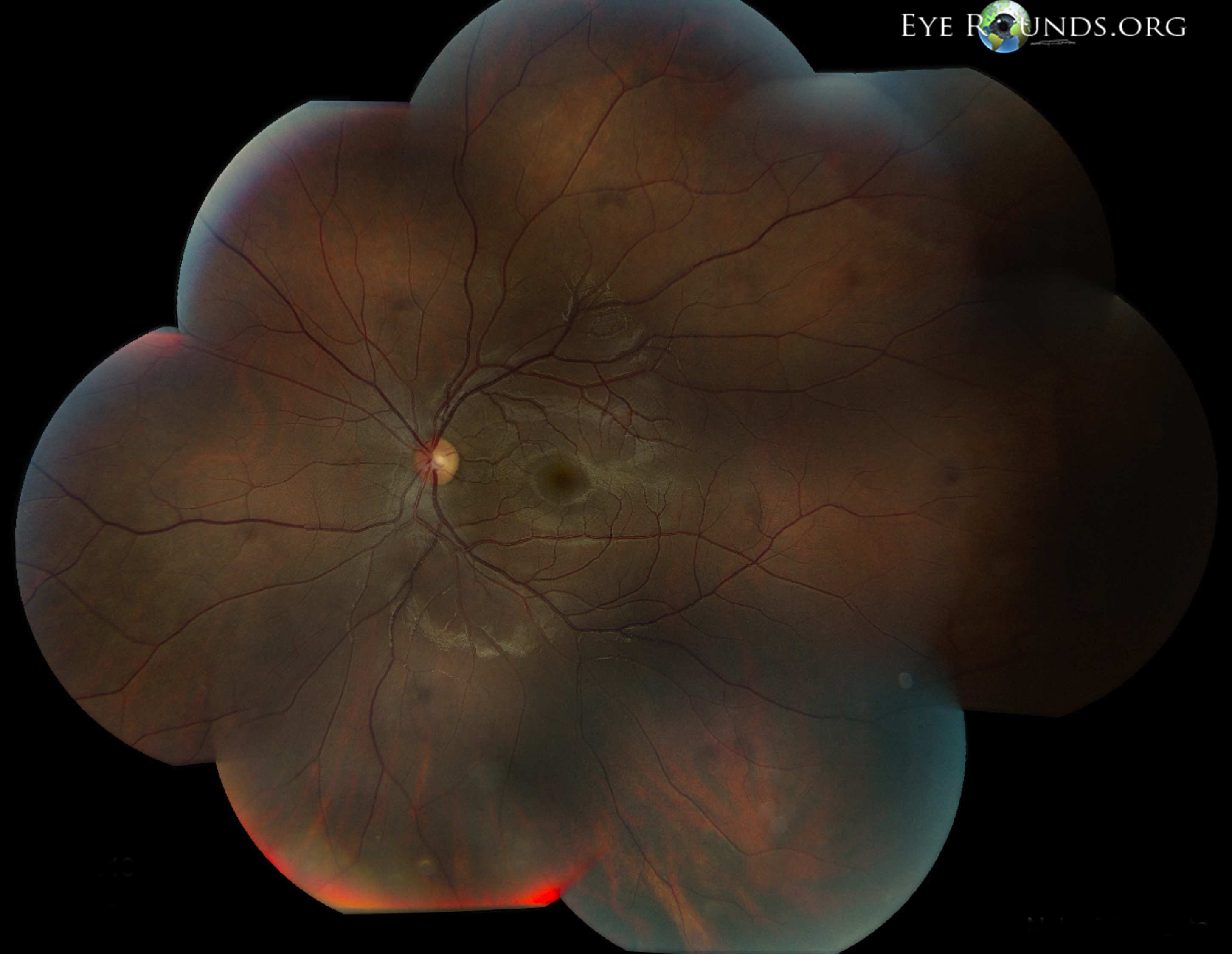
Toxoplasmic retinochoroiditis lesions have similar fundus characteristics, whether they result from congenital or acquired infections. Acute and new lesions are usually intensely white, focal lesions with overlying vitreous inflammatory haze. Active lesions with a severe vitreous inflammatory reaction will have the classic "headlight in the fog" appearance.[2]
Patients with active toxoplasmic retinochoroiditis may develop retinal vasculitis with vascular sheathing and hemorrhages in response to reactions between circulating antibodies and local Toxoplasma gondii antigens.[3]
Typically, hyperpigmented scars of old and inactive lesions are present with recurrent "satellite lesions" at the border of healed scar. As a lesion heals, its borders become more defined and hyperpigmented. Large scars will have an atrophic center devoid of all retinal and choroidal elements. The underlying sclera gives the lesion its white center.[4]
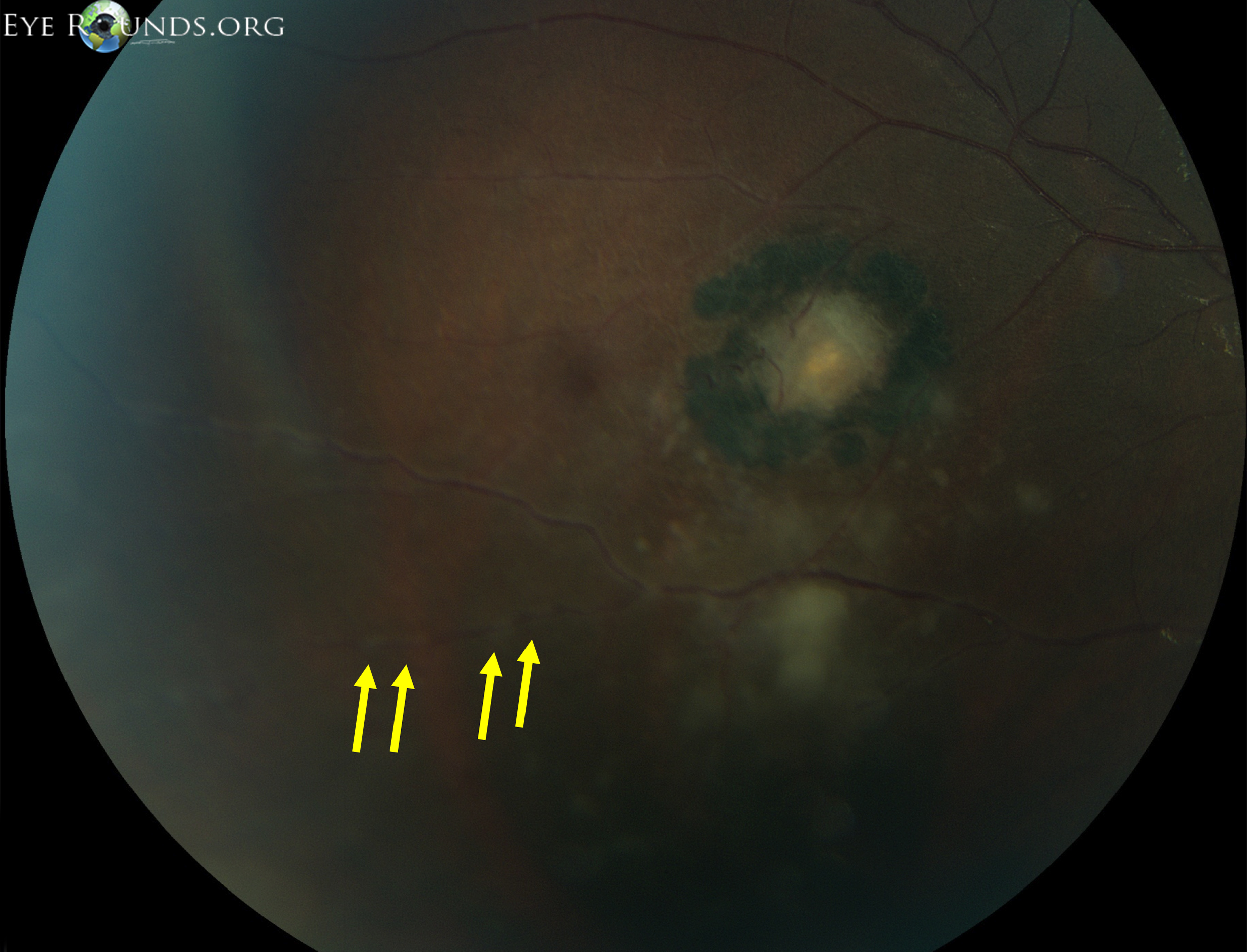
"Kyrieleis plaques" describe nodular peri-arteritis or a beaded pattern of vascular inflammation. These plaques are predominately associated with toxoplasmosis infections but were originally reported in association with ocular tuberculosis in 1933.[5] It may be less commonly seen with syphilis, tuberculosis, cytomegalovirus, herpes zoster, and others.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.