Chief Complaint: Visual disturbance when changing positions.
History of Present Illness: A 60-year-old male with a history of simple megalocornea presented to the Iowa City Veterans Administration Healthcare System eye clinic reporting visual disturbance while changing head position for several months. He noticed that his vision worsened with his head bent down. He previously had cataract surgery with an iris-sutured IOL due to the large size of his eye, which did not allow for placement of an anterior chamber intraocular lens (AC-IOL) or scleral-fixated lens.
Past Medical History: Megalocornea
Medications: None
Family History: No known history of megalocornea
Social History: None contributory
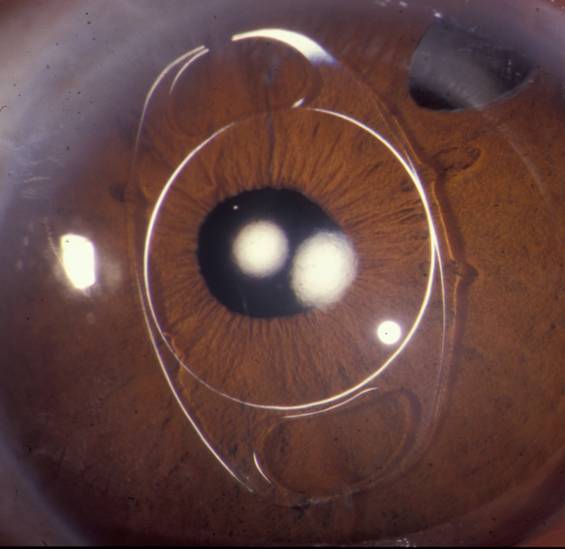
The patient’s iris-sutured IOL had become loose (tilted and de-centered) in his large anterior chamber, despite several sutures that had been placed in the past, resulting now in visual disturbance with movement. FDA and IRB approval was obtained to place an Artisan iris-clip IOL (Ophtec®). He was taken to the OR where his existing IOL was removed using Duet forceps and scissors. The Artisan IOL was placed using enclavation iris forceps. His postoperative course was unremarkable and his postoperative best-corrected visual acuity was 20/20. See video by Drs. Oetting and Privett for operative summary.
Megalocornea is a rare, inherited (predominantly X-linked) congenital disease characterized by nonprogressive bilateral enlargement of the corneal diameter to greater than 13 mm in the absence of elevated intraocular pressure. While the cornea itself is histologically normal, megalocornea has been associated with two patterns of presentation: 1) simple isolated megalocornea with no additional ocular or systemic manifestations and 2) megalocornea with other associated ocular and systemic abnormalities including megalophthalmos anterior and/or dysgenesis of the iris, lens, or ciliary body. A large cornea can also been seen in buphthalmos as in congenital glaucoma (diffuse enlargement of the eye) but is considered a separate disease and should not be confused with megalocornea.
The definitive cause of megalocornea is currently unknown. A number of mechanisms have been proposed including failure of anterior cup fusion during embryogenesis. It has been hypothesized that this allows more room for corneal growth during development (Mann, 1957). The findings of normal endothelial cell density and posterior placement of the iris-lens diaphragm seem to support the "cup fusion" theory. Embryologically, the cornea forms by growing anteriorly from its base near the ciliary ring. If the diameter of the ciliary ring is enlarged, the cornea will also be enlarged. In megalocornea, hyperplasia of the cornea is observed, which implies synchronous growth of all corneal layers and actively proliferating endothelial cells. Skuta and colleagues point out that this type of primary overgrowth in megalocornea results in normal endothelial cell density as opposed to decreased endothelial cell density, which would be seen in a cornea that was enlarged from secondary distension related to congenital glaucoma (Skuta, 1983).
Megalocornea is known to be a genetic disorder with over 90% of cases being X-linked recessive with a gene locus indentified in band Xq12-q26 (most likely q21-q23) (Meire, 1991, OMIM, 2000). As such, this is primarily a disease affecting males.
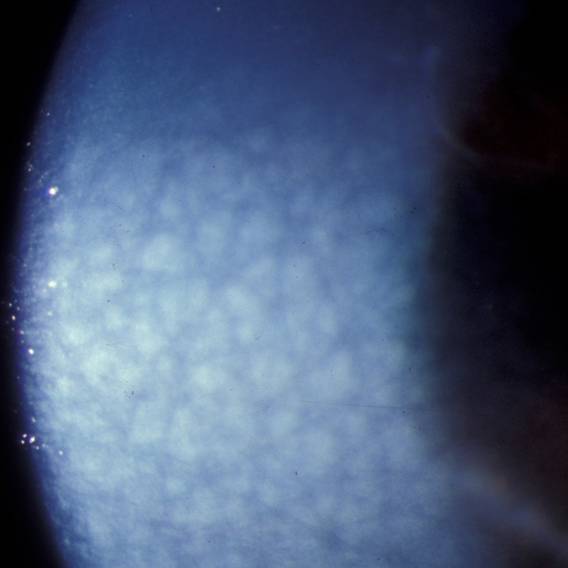
Physical findings of simple megalocornea include bilateral corneal enlargement most often between 13-16.5 mm, a dome-shaped cornea with normal thickness and occasional central mosaic dystrophy, increased anterior chamber depth, posterior positioning of the lens-iris diaphragm, shortened vitreous length, and normal intraocular pressure (Meire and Delleman, 1994).
Other key conditions in the differential diagnosis of congenital corneal enlargement include megalophthalmos anterior and primary congenital glaucoma (Table 1). One feature that distinguishes megalophthalmos anterior from megalocornea is widening of the ciliary body band such that it appears wider than the trabecular meshwork and scleral spur on gonioscopy (Kuchenbecker, 2002; Meire and Delleman, 1994). Other ocular abnormalities associated with megalophthalmos anterior include iridodonesis, iris stromal hypoplasia, phacodonesis, ectopia lentis, cataracts, and pigmentary glaucoma with Krukenberg spindles (Vail, 1931; Neumann, 1984; Javadi, 2000; Chien-Kuang, 2005; Vaz, 2007).
Findings that differentiate congenital glaucoma from megalocornea include elevated intraocular pressure, optic disc cupping, corneal edema, Haab’s striae (horizontal tears in Descemet’s membrane), increased axial eye length, decreased endothelial cell density, flattened cornea, and decreased lens thickness (Ho, 2004). It has also been noted that while megalocornea is extremely symmetric in presentation, congenital glaucoma can display asymmetry (Harley, 1983). Congenital glaucoma usually develops late in the fetus, and corneal findings are secondary to high intraocular pressure. In contrast, megalocornea is thought to be pre-determined at a much earlier embryologic period and corneal findings are due to primary corneal overgrowth (Meire, 1994).
Management of megalocornea depends on the degree of abnormality and the severity of associated ocular and systemic abnormalities. Simple megalocornea can be managed with routine correction of refractive error and consistent follow-up to monitor for cataracts and glaucoma. Megalocornea poses several challenges in the surgical management of cataracts. Enlargement of the ciliary ring and capsular bag in addition to weakened zonules makes standard placement of a routine PCIOL problematic. In such cases, there is a high likelihood of lens displacement within the capsule or posteriorly into the vitreous.
A number of surgical techniques have been developed to perform satisfactory intraocular lens (IOL) implantation in patients with megalocornea. Some innovations include posterior iris-sutured IOLs that include bites through the anterior capsule, posterior iris-clip IOLs, the iris-supported Binkhorst IOL, and anterior chamber IOLs with or without iris suturing (Neumann, 1984; Dua, 1999; Javadi, 2000; Basti, 2005; Vaz, 2007). Oetting and Newsom (2006) at the University of Iowa described the use of the Artisan IOL (Ophtec BV), which attaches to the iris via clips located on both sides of the optic. Such anchoring of the optic to the iris confers stability to the IOL position without having to rely on disease-altered anatomy.
Patients with megalocornea should be followed regularly for glaucoma and cataracts and screened for iris, lens, or ciliary body dysgenesis. Systemic conditions associated with megalocornea are numerous and include albinism, Alport syndrome, craniosynostosis, Down syndrome, Marfan syndrome, megalocornea-mental retardation syndrome, osteogenesis imperfecta and polycystic kidney syndrome among others (Roche, 2002). Diagnosis of megalocornea should trigger a developmental evaluation by a pediatrician. Overall, the prognosis of simple megalocornea is excellent.
| Simple Megalocornea | Anterior Megalophthalmos | Primary Infantile Glaucoma | |
|---|---|---|---|
| Inheritance | X-linked recessive | X-linked recessive | Sporadic |
| Age of presentation | Congenital | Congenital | First year |
| Natural History | Non-progressive | Non-progressive | Progressive |
| Symptoms | None | Variable based on clinical presentation | Photophobia; epiphora |
Physical Findings |
|||
| IOP | Normal | Normal | Elevated |
| Visual acuity | Variable | Variable | Myopia (Refractive from high axial length) |
| Corneal Exam | Cornea globosa; mosaic dystrophy (frequently) | Cornea globosa; mosaic dystrophy (frequently); Krukenberg spindle | Flattened cornea; buphthalmos; Haab striae; corneal edema; decreased endothelial cells |
| Corneal diameter | >13 mm; symmetric | >13 mm; symmetric | Variable; asymmetric |
| Axial length | Normal | Normal | Increased axial length |
| AC | Increased depth | Increased depth | Increased depth |
| Lens | Normal but increased propensity for cataract formation | Phacodonesis; ectopia lentis; increased propensity for cataract formation | Normal or decreased thickness |
| Lens-iris diaphragm | Posterior placement | Posterior placement; enlarged | Normal |
| Iris | Normal | Iridodonesis; iris stromal hypoplasia | Normal with high insertion |
| Vitreous | Decreased length | Decreased length | Increased length |
| Optic disc | Normal with increased propensity for glaucoma | Normal with increased propensity for glaucoma | Cupping |
 |
|---|
 |
|---|
 |
|---|
EPIDEMIOLOGY:
|
SIGNS:
|
SYMPTOMS:
|
TREATMENT:
NOTE: Children should be referred for an extensive developmental workup |
Basti S and Koch DD. Secondary peripheral iris suture fixation of an acrylic IOL in megalocornea. J Cataract Refract Surg 2005; 31(1):7.
Chien-Kuang et Al. Anterior Megalophthalmos. Chang Gung Med J 2005; 28:191-195.
Dua HS et Al. Cataract extraction and intraocular lens implantation in anterior megalophthalmos. J Cataract Refract Surg 1999; 25:716-719.
Harley R. Abnormalities of corneal size and shape: Megalocornea and anterior megalophthalmos. In: Pediatric Ophthalmology. Philadelphia: W.B. Saunders, 1983: 468-471.
Ho CL and Walton DS. Primary Megalocornea: clinical features for differentiation from infantile glaucoma. J Pediatr Ophthalmol Strabismus 2004; 41(1):11-17.
Javadi MA et Al. Cataract surgery and intraocular lens implantation in anterior megalophthalmos. J Cataract Refract Surg 2000; 26:1687-1690.
Kraft SP et Al. Megalocornea: a clinical and echographic study of an autosomal dominant pedigree. J Pediatr Ophthalmol Strabismus 1984; 21:190-193.
Kuchenbecker J and Behrens-Baumann W. Ciliary body dysplasia in megalohthalmos anterior diagnosed using ultrasound biomicroscopy. Nature 2002; 16(5):638-9.
Mann I. Developmental abnormalities of the eye, 2nd ed. Philadelphia: J.B.Lippincott Co., 1957, pp. 251-253,352
Meire FM. Megalocornea. Clinical and genetic aspects. Doc Ophthalmol 1994; 87:46-52.
Meire FM and Delleman JW. Autosomal dominant congenital meiosis with megalocornea. Ophthalmic Paediatr Genet 1992; 13:123-129.
Meire FM and Delleman JW. Biometry in X linked Megalocornea: pathognomonic findings. British Journal of Ophthalmology 1994; 78:781-785.
Meire FM et Al. X-linked Megalocornea. Ocular finding and linkage analysis. Ophthalmic Paediatr Genet 1991; 12(3):153-157.
Neumann AC. Anterior megalophthalmos and intraocular lens implantation. J Am Intraocul Implant Soc. 1984; 10(2):220-222.
Oetting TA and Hendrix MA. Megalocornea. eMedicine Ophthalmology. Last updated May 2010. <http://emedicine.medscape.com/article/1196299-overview>.
Oetting TA and Newsom TH. Bilateral Artisan lens for aphakia and megalocornea: Long-term follow-up. J Cataract Refract Surg 2006; 32(3):526-528.
OMIM. Online Mendelian Inheritance in Man, OMIM(TM). McKusick-Nathans Institute for Genetic Medicine, Johns Hopkins University (Baltimore, MD) and National Center for Biotechnology Information, National Library of Medicine (Bethesda, MD), 2000. Available at: http://www.ncbi.nlm.gov/Omim/.
Roche et Al. Congenital Megalocornea. J Fr Ophthalmol 2002; 25(3):312-318.
Skuta GL et Al. Corneal endothelial cell measurements in megalocornea. Arch Ophthalmol 1983; 101(1):51-3.
Vail DT. Adult hereditary anterior megalophthalmos sine glaucoma: a definite disease entity, with special reference to extraction of the cataract. Arch Ophthalmol 1931; 6: 39.
Vaz FM and Osher RH. Cataract surgery and anterior megalophthalmos: Custom intraocular lens and special considerations. J Cataract Refract Surg 2007; 33(12):2147-2150.
Welder J, Oetting TA. Megalocornea. EyeRounds.org. Sept 17, 2010; Available from: http://www.EyeRounds.org/cases/121-megalocornea.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.