Chief Complaint: Eye crossing
History of Present Illness: The patient is a 4-year-old boy who originally presented to an outside ophthalmologist at 2 years of age after his parents noted that his eyes were crossing. The crossing was first noted a few weeks prior to that visit. He was evaluated and placed in glasses, which resulted in partial improvement of the crossing. Over the ensuing 2 years his prescription was updated as needed by the outside provider. His mother seeks a second opinion to ensure that his condition is being managed appropriately. The mother reports that the patient wears his glasses well. She sees occasional crossing with the glasses on. He has never been patched. He is otherwise healthy, growing and developing normally.
He was born full term by normal spontaneous vaginal delivery without complications.
None
No known strabismus or inherited eye disease
Pupils: Equally round and briskly reactive. No relative afferent pupillary defect.
Stereopsis testing: Unable to test
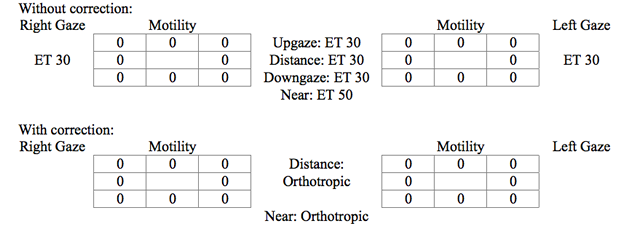
Strabismus exam: Alternate Cover Testing
Slit lamp exam: Within normal limits OU
Dilated fundus exam: Within normal limits OU
Visual acuity with correction: HOTV
Pupils: Equally round and briskly reactive. No relative afferent pupillary defect.
Stereopsis testing*:
Strabismus exam: Alternate Prism Cover Test
General: Normal mood and behavior; no nystagmus or abnormal head position
Slit lamp exam: Normal OU
Dilated fundus exam: Normal macula, vessels and periphery OU. Cup to disc ratio 0.2 OU.
Diagnosis: Refractive Accommodative Esotropia
Accommodative esotropia is defined as the convergent deviation of the eyes associated with activation of the accommodative reflex. It is classically divided into three categories:
Accommodative esotropia is the most common cause of childhood esotropia.
These esodeviations share common characteristics. All accommodative esodeviations are acquired with onset generally between 6 months and 7 years of age, with average onset at 2.5 years of age. Rare cases have been reported from age 3 months to 11 years old. At the onset, the deviation is usually intermittent, but usually becomes constant in the following weeks to months. It is not uncommon to obtain a history of illness, trauma or fatigue as a precipitating factor for the onset of the deviation. There often is a family history of strabismus. Studies suggest that approximately 77% of patients with accommodative esotropia have a first- or second-degree relative with the same condition. Among first-degree relatives alone, the prevalence of accommodative esotropia is 23%; therefore, it is important to have siblings examined. These esodeviations are frequently associated with amblyopia (Hutchison 2004).
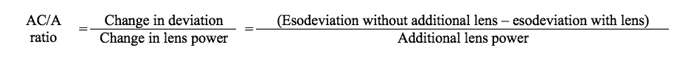
All children with new-onset esotropia require a thorough history, review of systems, and comprehensive examination. The examination must include assessment of vision, ocular motility, strabismus measurements at distance and near and cycloplegic refraction in addition to a general ocular examination. Distance and near measurements are essential to determine the accommodative convergence to accommodation (AC/A) ratio. The AC/A ratio should be investigated if there is good alignment in the distance and greater than 10 prism diopters of increased esodeviation at near in full correction. The next step is to relax accommodation and determine the remaining amount of convergence. We typically hold +3.00 diopter lenses over both eyes and remeasure the esodeviation at near. The esodeviation while looking through +3.00 D lenses is subtracted from the original esodeviation at near without the +3.00 D lenses and the difference is divided by +3.00. If the value is greater than 5, then the patient has a high AC/A ratio. The treatment in this setting may include bifocals if they allow the patient to fuse.
Calculation of Accommodative Convergence/Accommodation (AC/A) ratio by the gradient method (measurements with and without the additional lens are done at the same distance):
This case is an example of refractive accommodative esotropia with normal AC/A ratio (in proper correction, the patient is orthophoric in the distance and at near). The mechanism of this type of esodeviation involves 3 factors:
The uncorrected hyperopia forces the patient to exert excessive accommodation to focus images on the retina, thus evoking increased convergence. If the patient’s fusional divergence mechanism is insufficient to compensate the increased convergence, esotropia results. Generally, in refractive accommodative esotropia, the deviation is between 20 and 30 prism diopters, the deviation is similar in the distance and at near, and the average amount of hyperopia is +4 diopters (range +3.00 to +10.00 diopters) (BCSC Pediatrics and Strabismus, 2007).
The goals of treating this condition are to restore normal ocular alignment, maintain good visual acuity in each eye, and promote good binocular function. Treatment consists of prescribing spectacle correction with the full amount of hyperopic correction as determined by cycloplegic retinoscopy. Significant delay in the initial treatment following the onset of esotropia increases the likelihood that a nonaccommodative component (partially accommodative esotropia) may develop (Mulvihill et al 2000). Of course, if there is any concurrent amblyopia, treatment should be initiated to address this issue.
To the ophthalmologist, the clinical diagnosis and treatment seems straightforward, but to the parent or caretaker the condition may not be as easily understood. Many parents often request surgery, thinking it will be a "quick fix." For the typical refractive accommodative esotropia patient, the treatment is glasses, not surgery. Strabismus surgery is indicated if optical correction is ineffective in restoring normal ocular alignment. It is important for the eye care provider to take the time to discuss the mechanism of the condition so that the child’s caretaker can comprehend the situation and fully cooperate with the treatment. The importance of full-time glasses wear and amblyopia treatment, if applicable, cannot be over-emphasized. To prevent frustration or misunderstanding, one should mention that the eyes will cross when the child is not wearing glasses because glasses control the deviation and do not cure it. It is also important to convey to the caretaker that this is a long-term condition that requires routine monitoring for amblyopia and that changes in spectacle prescription may be required not only to maintain vision but also alignment. Parents are also frequently concerned over their child’s long-term prognosis. Although the child’s course cannot be predicted at the initial visit or even within years of initiating treatment, it is often helpful to mention that some children can be weaned out of their glasses, while others will require optical correction to maintain alignment throughout adulthood. Contact lenses and refractive surgical procedures may be options as the child nears adulthood.
Summary
|
Signs
|
Symptoms
|
Treatment
|
Hutcheson KA. Childhood esotropia. Curr Opin Ophthalmol 2004;15(5):444-8.
"Refractive Accommodative Esotropia" in Chapter 7: Esodeviations. Basic and Clinical Science Course: Section 6. Pediatric Ophthalmology and Strabismus. San Francisco: American Academy of Ophthalmology, 2010-2011:93-95.
Mulvihill A, MacCann A, Flitcroft I, O'Keefe M. Outcome in refractive accommodative esotropia. Br J Ophthalmol 2000;84(7):746-9.
*Please see https://eyerounds.org/tutorials/Bhola-BinocularVision.htm for a more in depth discussion about binocular vision.
Rogers GM, Longmuir SQ. Refractive Accommodative Esotropia. EyeRounds.org. January 26, 2011; Available from: https://eyerounds.org/cases/129-accommodative-esotropia.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.