Chief Complaint: 57-year-old white female with 1 day history of redness, swelling, and pain in her right eye.
Ocular History:
Medical History: Emphysema, angina, diverticulitis, gallstones, GERD
Ocular Exam: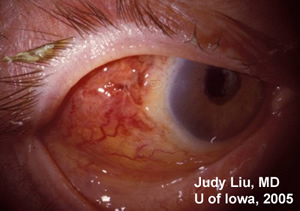 |
 |
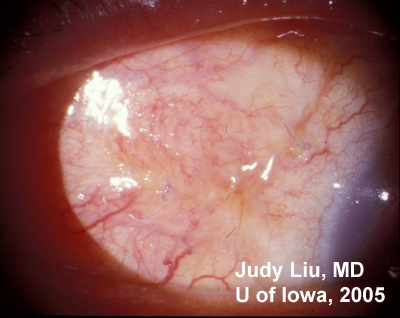
| 1A: Slit lamp view of the injected, chemotic conjuntivae overlying the Ahmed device, OD. | 1B: Fundus, OD. Large cup to disc ratio, but no vitreous cell and otherwise normal fundus. (The yellow crescent is photographic artifact). |
Labs: Complete blood count (CBC) and metabolic panel were both normal. Blood cultures were negative.
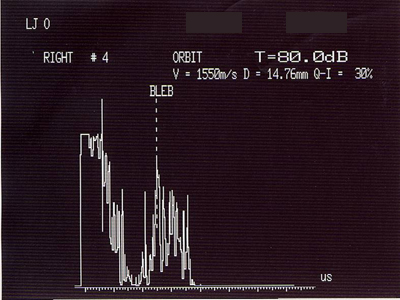
A painful, red, proptotic eye led us to be concerned about infection. Suspecting involvement of the glaucoma drain (implanted seton), a B-scan (echo) of the orbit and lids was performed, OD. This showed a bleb twice the normal size filled with turbid fluid (see Figure 2).
 |
A computed tomography (CT) scan of the orbit and sinuses was performed and is shown in Figure 3.
 |
Our patient presented with acute red eye, pain and decreased vision. Clinical picture, combined with echo and CT scan of the orbit, confirmed a diagnosis of orbital cellulitis associated with the Ahmed seton, and possibly the scleral buckle. In this case, there was no associated intraocular infection. Broad-spectrum intravenous antibiotics (vancomycin and ceftriaxone) were started with prompt surgical removal of the Ahmed seton and scleral buckle on the day of presentation.
Mucopurulent material found upon opening the tenons capsule around the seton bleb was drained and sent for culture. Gram stain initially revealed gram negative bacilli (see Figure 4) and cultures grew Serratia marcescens from both her extracted seton and scleral buckle element. Some colonies of Enterococcus grew from samples of the scleral buckle only.
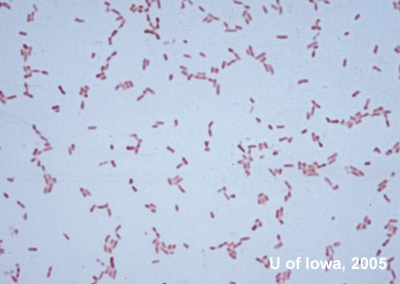 |
Serratia marcescens has been identified as the causative agent in lacrimal duct infections, conjunctivitis, keratitis, and endophthalmitis. Frequently, the infection has been associated with systemic risk factors such as diabetes mellitus, renal failure, alcoholism, and rheumatoid arthritis. S marcescens can be found not uncommonly in the respiratory and urinary tract in adults and within the gastrointestinal system of young children. S marcescens ocular infections have been associated with contact lens wear, especially rigid gas-permeable contact lenses and previous eye surgery.
Enterococcus, the second organism cultured from the scleral buckle, is a part of the normal fecal flora and can cause eye infections including endophthalmitis, orbital cellulitis from sinus disease, and keratitis. It is an uncommon cause of scleral buckle-related infection. In one case series from Bascom Palmer, Enterococcus (Streptococcus fecalis) was found in only 6% of positive cultures.
In our patient, there were no identifiable systemic risk factors. However, her ocular risk factors included contact lens wear and previous eye surgeries. In this case, the patient's contact lens was suspected as the source of infection, and we were able to culture Serratia directly from it. It is unclear how the organisms gained access to the seton and bleb without evidence of a breach of the conjunctiva. It is possible that use of mitomycin C may have thinned the conjunctiva over the seton bleb facilitating microbial access. Despite severe orbital infection, there was no sign of endophthalmitis (as witnessed by clear anterior chamber and clear vitreous media noted in the exam above). This is consistent with the idea that the Ahmed seton functions like a one-way valve and does not allow backflow from the orbit into the eye.
The treatment of S marcescens ocular infection is challenging because the organism is multi-drug resistant. Aminoglycosides and amikacin both show consistent efficacy in vitro. Third generation cephalosporins, fluoroquinolones, trimethoprim/sulfamethoxazole, tetracycline, and synthetic penicillins show more variable activity. In our patient, IV ceftriaxone followed by a 2 week course of oral levofloxacin was effective (post-operative image in Figure 5). Antibiotic resistance is also a problem in the treatment of Enterococcus, but vancomycin is frequently effective.
S marcescens is a rare cause of orbital cellulitis, but a potentially sight-threatening one if it is not detected early and treated aggressively. A high index of suspicion and prompt managment can lead to good visual outcomes.
 |
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Liu J, Kwon YH. Seton Infection: Serratia Marcescens: 57-year-old white female with 1 day history of redness, swelling, and pain in her right eye. EyeRounds.org. March 5, 2005; Available from: http://www.EyeRounds.org/cases/34-setoninfection.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.