Chief Complaint: 30-year-old male presents with a history of migraine headaches associated on two occasions with diplopia lasting for 2-4 weeks.
History of Present Illness: At presentation, the patient describes a history of 2 weeks of headache after which he noted diplopia, an asymmetrically dilated pupil as well as mild ptosis in the right eye. He described the pain at the onset of the headache as 10 out of 10 in intensity and it was associated with photophobia and nausea. He had used some acetaminophen, but had no improvement with this headache. He reported that the headache was getting better and his diplopia had resolved. However, he still felt that his right lid was still a little lower than the left. Presently, he ranks his pain at 2/10 on the pain scale.
Past Ocular History: He reports that at age five he experienced three weeks duration of ophthalmoplegia in the right eye with ptosis, dilated pupil, and accompanying severe headache.
Medical History: At the time of the recent ophthalmoplegia, headache and ptosis, he underwent cerebral angiography at an outside facility to rule out aneurysm, which was normal. He has had classic migraine headaches with photophobia and nausea for many years.
Medications: Acetaminophen, as needed, with no relief of symptoms.
Family History: Noncontributory
Social History: He drinks about 1-2 alcoholic beverages per week and has a 7.5 pk/yr history of cigarette smoking (1/2 pack/day for 15 years).
Exam, Ocular:
 |
 |
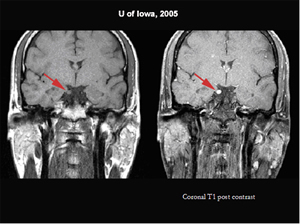
Course: As a child, at age 5, the patient had already undergone normal imaging of the brain. Now, with repeated headaches and ophthalmoplegia, repeat MRI was performed. This showed enhancement of cranial nerve III on the right (see Figures 3 and 4), but no other abnormality of the brain, brainstem, or orbit. Differential diagnosis of an enhancing enlarged third nerve includes schwannoma, granulomatous disease and ophthalmoplegic migraine. Cerebral angiography had already ruled out concern for aneurysm. Given the present and past association of a third nerve palsy with severe migraine in a child and as a young adult, followed by resolution within weeks, it was felt that the patient most likely had ophthalmoplegic migraines. This entity has been reported to be associated with enhancement of the third nerve on MRI scans. He was referred to the Neurology headache service for treatment options. The Neurology service agreed and started the patient on a trial of Verapamil for migraine prevention, which helped to alleviate his symptoms.
| Figure 3: Coronal T1 MRI without contrast and with contrast on the right. There is an enhancing enlargement of the third nerve. | Figure 4: Axial MRI T-1 images without and with contrast. The MRI shows the enlargement and enhancement in the cisternal portion of the right third cranial nerve. |
 |
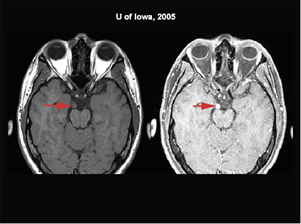 |
Based on his examination findings of mild residual right 3rd nerve palsy with mild pupil involvement, slight ptosis of the right eye and the MRI which showed an enlarged enhancing right third nerve at its exit from the brainstem, the differential included ophthalmoplegic migraine, schwannoma or granulomatous disease. Schwannoma is less likely the diagnosis since his diplopia had been episodic and recovered; in cases of schwannoma, there is a slowly progressive weakness of the third nerve over years. Granulomatous disease such as sarcoidosis or Tolosa Hunt syndrome can cause a pupil involving 3rd nerve palsy but these usually occur in adults, are associated with retro-orbital pain and are slow to resolve, especially without prednisone treatment. Tolosa Hunt syndrome is usually associated with meningeal enhancement on MRI scans. The prior history of a third nerve palsy at age 5 , which resolved sponaneously and whose onset was associated with headache also made ophthalmoplegic migraine more likely.
Ophthalmoplegic migraine is a rare condition, which is characterized by localized headache in the orbital region associated with partial or complete paralysis of the oculomotor nerve. Classically, ophthalmoplegic migraine involves recurrent headache attacks with migrainous characteristics associated with paresis of one or more ocular cranial nerves in the absence of any demonstrable intracranial lesion other than MRI changes within the affected nerve. The pathophysiology remains unclear and possible etiologies that have been suggested are ischemia, compression secondary to vascular anomaly, and inflammation. Enhancement of the third nerve on MRI can also occur in both infectious and non-infections inflammatory conditions. Non-infectious causes of cranial nerve enhancement that have been suggested are similar to the Tolosa-Hunt syndrome occurring in the interpeduncular segment of the third nerve and also sarcoidosis, and are usually associated with meningeal enhancement. Resolution of these conditions is usually achieved with steroid therapy. The demonstration on MRI of thickening and enhancement of the cisternal part of the oculomotor nerve has prompted others to consider it a recurrent demyelinating neuropathy. MRI enhancing cisternal portions of the third nerve can also occur in neoplastic conditions such as schwannomas or hemangiomas which are benign and in malignant conditions such as lymphoma, malignant glioma, leukemia, and carcinomatous meningitis. However, none of these neoplastic conditions resolve spontaneously. When there is enhancement of third nerve on MR images, further imaging may not be necessary, but careful clinical evaluation with spinal tap are necessary to rule out lymphoma, leukemia, or infectious disorders. If work-up is negative, a diagnosis of ophthalmoplegic migraine may be made. If there is no enhancement of the third nerve, then further radiological testing is necessary including angiography to rule out aneurysm.
Ophthalmoplegic migraine generally first occurs in childhood, with repeated episodes occurring in adulthood. The prognosis is good, with resolution of the third nerve paresis, but with repeated attacks, residual deficits of the third nerve may remain. Migraine prophylactic medications such as beta-blockers and calcium channel blockers have been proposed for ophthalmoplegic migraine. Steroids have been used, but efficacy has not been proven.Diagnosis: Ophthalmoplegic Migraine
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Quisling S, Kardon RH: Ophthalmoplegic Migraine: 30-year-old male with migraine headaches and occasional diplopia. Eyerounds.org. March 7, 2006; Available from: http://www.EyeRounds.org/cases/52-Opthalmoplegic-Migraine-Diplopia-Headache.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.