Chief Complaint: Decreased distance visual acuity for four months.
History of Present Illness: The patient is an eight-year-old white male who suffers from seasonal allergic rhinitis. He presents for an eye examination complaining of a four month history of decreased distance visual acuity. Of note, he has a history of phlyctenulosis superiorly in the right eye during the previous summer that resolved with lotepredonol 0.5% topical therapy.
Past Ocular History: Unremarkable for surgery or trauma. He is mildly myopic with a current optical prescription of -1.75 spherical in both eyes (OU). Phlyctenulosis as noted above.
Medical History: History of asthma and seasonal allergies throughout his childhood.
Medications: His allergic rhinitis is treated with beclomethasone dipropionate nasal spray (Vanceril) and combined oral therapy of chlorpheniramine and pseudoephedrine (Kronofed, antihistamine and decongestant).
Family History: Maternal grandparent with cataract, glaucoma and macular degeneration. Multiple myopic family members.
Social History: The patient is a well-adjusted 2nd-grader who lives at home with his parents. He has had no known exposure to anyone with infectious eye disease.
Ocular Examination: Moderate photophobia noted during the exam.
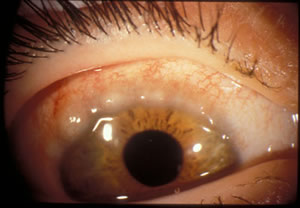
| Figure 1: OD - Broad, gelatinous, thickened, opacified, mucoid nodular infiltrates of eosinophils and epithelial debris. Horner-Trantas Dots (punctiform calcified concretions) are at the apices of the nodules. | Figure 2: OS - Limbal conjunctivitis: broad, gelatinous, thickened, opacification of superior limbus. |
 |
 |
Course: The patient's course and presentation is classic for vernal keratoconjunctivitis. The day of presentation, the patient was started on the topical steroid Lotomax (loteprednol etabonate 0.5%) BID and the topical antihistamine Optivar (azelastine 0.05%) BID. At his 1 week follow-up visit, the limbal and palpebral signs were resolving. The Lotamax was tapered off. At his 6 week follow-up, there was no sign of limbal involvement of disease and only mild papillae of the tarsal conjunctiva. The patient was continued on Optivar until symptoms resolved.
Discussion: Vernal keratoconjunctivitis (VKC) is an allergy associated recurrent inflammatory disease found predominately in prepubescent males. It is characterized by the bilateral presence of palpebral and/or bulbar conjunctiva papillae, corneal keratopathy and mild to severe itching. The predominant age range is 5 to 20 years, with a peak incidence at 11 to 13. Young males are affected twice as often as young females. There is a higher predilection for warm, dry climates, as inflammation trends decrease in the cooler months of the year. Incidence increases with a family history positive for atopic disease (asthma, rhinitis, and eczema). Vernal keratoconjuctivitis is self-limiting and typically lasts 4-10 years with remission at puberty. The immunopathogenesis is multifactorial. Classically it has been thought of as a type I IgE-mediated hypersensitivity reaction, however it has been suggested that there is cell-mediated Th-2 involvement.
The major symptom is ocular itching. Minor symptoms include: photophobia, burning, tearing, mild ptosis and a thick, ropy, yellow, mucoid discharge. Clinically, there are three forms of conjunctivitis: palpebral, limbal and mixed. The palpebral form is characterized by polygonal, flat-topped, giant cobblestone papillae of the superior tarsal conjunctiva. The limbal form is less common and marked by a broad, thickened, opacification of the superior limbus. The tissue is composed of lymphocytes, plasma cells, macrophages, basophils and a high level of eosinophils. The characteristic Horner-Trantas dots are white dots of eosinophils and epithelial debris. There is corneal involvement in half of cases that range from punctuate epithelial keratitis to superficial pannus to corneal shield (Togby’s) ulcers. Corneal ulcers are observed in 10% of patients. The diagnosis of VKC is made clinically, based on history and ocular examination. Conjunctival scrapings, exhibiting eosinophils can help confirm, but is not necessary, for diagnosis.
Complications of visual loss from corneal neovascularization, corneal scars, keratoconus and steroid induced cataracts and glaucoma are found in 6% of patients. Increased size of papillae and the bulbar form of conjunctivitis exhibit poorer prognosis and result in a higher complication rate.
Treatment: Management is aimed at minimizing inflammation until the disease naturally subsides. Pharmacologic therapy is the mainstay of treatment. Topical treatments are more effective than systemic. The first-line of treatment is a topical mast cell stabilizer, antihistamine or mast cell stabilizer/antihistamine combination (olopatadine or lodoxamide). These classes of drugs are safely used long-term for moderate to severe cases and should be taken one month prior to the seasonal onset of symptoms. Steroid use is limited to severe inflammation and corneal shield ulcers to minimize iatrogenic harm. Cases not responding to steroids can be treated with cyclosporine. Nonsteroidal anti-inflammatory eye drops are used as a safe alternative in mild cases. Environmental strategies of therapy include: avoidance of allergens and triggering factors, cold compresses and moving to a cooler climate.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT4 weeks prior to allergy season begin topical treatment with:
If severe inflammation or shield ulcer is present:
If not responding to treatment, consider cyclosporine 0.05% BID |
Koczman J, Oetting TA: Vernal Keratoconjunctivitis: 8-year-old asthmatic male with reduced vision. EyeRounds.org. June 25, 2007; Available from: http://www.EyeRounds.org/cases/70-Vernal-Keratoconjunctivitis-Atopic-Asthma.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.