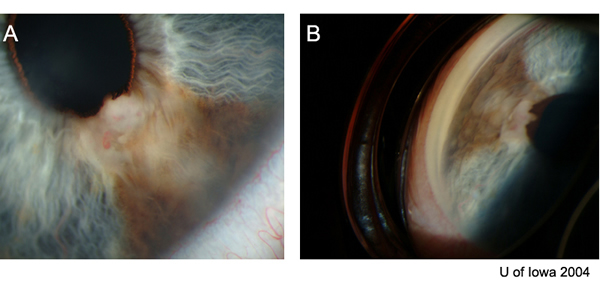
Chief Complaint: 47-year-old male referred in 1997 for evaluation of iris lesion OS.
History of Present Illness: Lesion OS was first noticed in 1972. The patient noted increased pigmentation. He was evaluated in 1997 at the University of Iowa, and it was decided to watch this lesion. There was slow, progressive growth of a pigmented, iris lesion OS in 2004. There are no other ocular complaints or visual problems.
PMH/FH/POH: Non-contributory.
 |
 |
 |
|
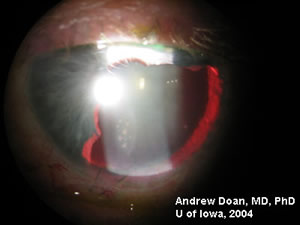
Video showing the removal of the iris lesion. If video fails to load, download Video in Windows Media Format Surgery performed by Wallace Alward, MD; Assisted by Thomas Weingeist, MD, PhD |
|
 |
 |
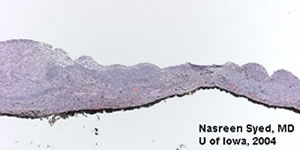 |
Low power view of excised iris tissue containing melanoma. |
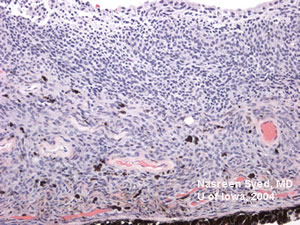 |
100X view of tumor containing both melanoma and nevus cells. Cells are invasive, pigmented, and form nests. |
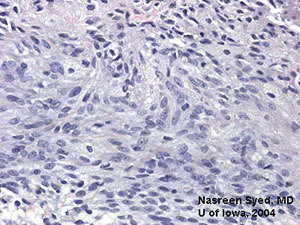 |
200X view of tumor, processed with bleach to remove melanin. Note large, vacuolated nuclei. Cellular structure shows atypia. |
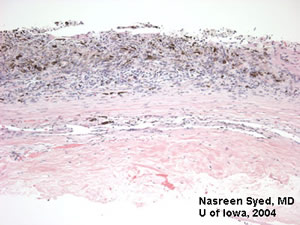 |
Slide showing that the tumor does not invade through sclera. |
The iris is an uncommon primary location for melanoma. Within uveal tissue, the most common locations for melanoma are (in descending order): choroid, ciliary body, and iris. Iris melanomas comprise 3-12% of uveal melanomas. The annual incidence is approximately 1/million.
Risk factors include Caucasian race and light iris color. Questionable risk factors include neurofibromatosis type-1 (NF-1) and sunlight exposure. The great majority of iris melanomas occur on the inferior half of the iris, which further implicates sun exposure.
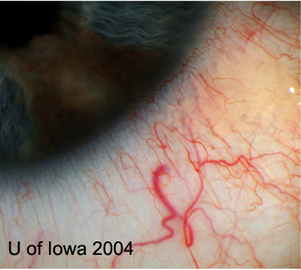
Patients present in a variety of ways. Usually, the patient or ophthalmologist notes a spot on the iris which grows over time. Less common presenting signs and symptoms include increased IOP, decreased vision, and hyphema.
Iris melanomas display a variety of growth patterns. Two main categories include nodular or diffuse growth patterns. "Ring melanoma" is a term used to describe a tumor which grows around the iris in a circular shape. These tumors usually display the diffuse growth pattern. Iris melanomas can be divided into 3 histologic types: Spindle B, Epithelioid, and Mixed. Spindle B is the most common type.
Iris melanomas may present with elevated IOP, although the majority do not. Causes of increased IOP are controversial, but include the following:
Elevated IOP can be treated by topical or oral medications. Treatment of the iris melanoma may help reduce IOP as well. Performing argon laser trabeculoplasty (ALT) is controversial, since it could cause dispersion of tumor cells. Some authors have suggested performing ALT well away from the tumor. Cyclodestructive procedures are also controversial. Filtration surgeries are contraindicated, because they have been associated with metastasis.
Differentiating benign iris nevi from malignant iris melanomas can be difficult. Multiple studies have sought to clarify risk factors for malignancy, which include:
However, although the above risk factors are suggestive of malignancy, many of the features may be seen in some iris nevi. The following may be seen in iris nevi, and have led to enucleation in some cases:
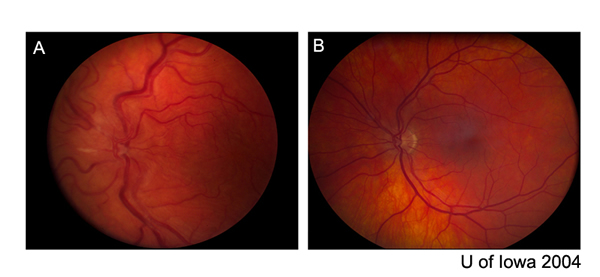
Metastasis is unusual in iris melanoma. The overall rate of spread at 10 years is 3-5%. Epithelioid tumors show a slightly higher rate (7%), while mixed tumors show the highest rate (11%). This is in contrast to choroidal melanomas, which metastasize most readily if epithelioid.
The true metastatic rate for iris melanoma is probably lower. Studies documenting metastatic rate include only patients with biopsy-confirmed tumors. Many patients may have slow growing iris melanomas that are mistaken for nevi, or not recognized at all. Other patients have slow growing lesions which are thought to be iris melanomas, but are followed long term and never undergo biopsy. Therefore, it is likely that the above studies select for the most aggressive tumors.
Metastatic rate for iris melanoma is lower than ciliary body melanoma, and much lower than choroidal melanoma. When metastases do occur, the liver and lungs are the most common sites.
Studies have sought to identify risk factors for metastasis:
Diagnosis can be difficult due to aggressive features which can occasionally be demonstrated by benign nevi. The following are diagnostic options:
Enucleation could be considered in eyes with poor vision. One example is an eye with intractable IOP rise. FNA is not associated with increased risk of metastasis. However, in a tumor composed of both nevus and melanoma cells, the FNA may pick up only nevus cells. Furthermore, in a small, slow-growing tumor distant from the angle, FNA may not change management. Excisional biopsy may be considered for smaller lesions.
It is important to consider that an apparent iris melanoma may simply be an extension of a choroidal or ciliary body melanoma. Ultrasound biomicroscopy can be particularly useful to investigate this.
Plaque radiotherapy is the newest treatment for iris melanoma. Because of the anterior location of iris melanoma, radiation retinopathy is not common after treatment. Cataract and iritis are the most common adverse reactions of radiotherapy.
Our patient decided to have an iridocyclectomy (see video) to remove the melanoma completely. The patient should be examined for recurrence and undergo yearly monitoring of liver function tests and chest X-rays.
EPIDEMIOLOGY
Risks factors for metastasis
|
SIGNS OF MALIGNANCY
|
SYMPTOMS
|
TREATMENT
|
Tantri A, Alward WLM, Weingeist TA. Iris Melanoma: 47-year-old male referred in 1997 for evaluation of iris lesion OS. EyeRounds.org. February 21, 2005; Available from: http://www.EyeRounds.org/cases/case25.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.