Chief Complaint: 60-year-old male who was evaluated 1 wk ago for "conjunctivitis" OS by internal medicine.
History of Present Illness: Patient complained of a painless, gradual redness of his left eye over the last several months. He does not report any pain, discharge, discomfort, or itching. He presented to the on-call ophthalmologist for evaluation. He pointed to some fullness of the superior aspect of the medial canthus OS with mild conjunctival injection. Pt also complained that things were "blurry" with a slight double image, which resolved when one eye was closed separately.
PMH: h/o non-Hodkin's lymphoma and in remission for numerous years. No other ocular history or medical problems. No h/o of ocular traumas or surgeries.
EXAM
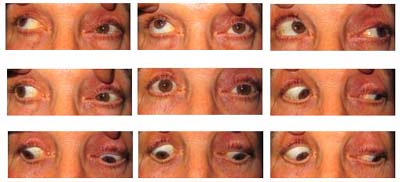
Figure 2: Left eye with superior conjunctival injection.
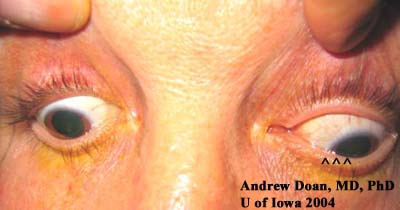
Figure 3: Left medial canthus with fullness. Note the asymmetric ptosis OS (more ptosis medially).

Coronal CT without contrast. |
Axial CT without contrast. |
| Note: large medial mass indenting globe | Note: large medial mass displacing medial rectus but is not eroding into bone or surrounding soft tissue. |
 |
 |
Figure 5: Anterior orbitotomy. Note the fleshy mass in the superior-nasal quadrant.

This patient presented with acute awareness of a long-standing problem: fullness of upper lid, binocular diplopia, and injection OS. He was diagnosed previously with "conjunctivitis" because of the asymmetric injection OS; however, he did not have other signs of infection: pain, itching, tearing, or discharge. On exam, his asymmetric ptosis OS (i.e. mechanical ptosis), elevation deficit OS on versions, proptosis OS, and a firm palpable mass in the superior-nasal quadrant OS should raise the suspicion of an orbital mass. In a patient with a history of non-Hodkin's lymphoma, orbital spread needs to be ruled out. The CT scans clearly denote a large orbital mass that is molding surrounding structures but not eroding into them.
An anterior orbitotomy was notable for a large, pink mass. Pathology confirmed the mass to be positive CD20 and BCL-2 lymphoma. Extensive imaging studies of head and body did not reveal additional tumor. The patient was treated by radiation oncology with local radiation.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Differential Diagnoses
Doan A, Oetting TA: Verticillata: Orbital Lymphoma: 60-year-old male who was evaluated 1 wk ago for "conjunctivitis" OS by internal medicine. February 21, 2005; Available from: http://www.EyeRounds.org/cases/case9.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.