
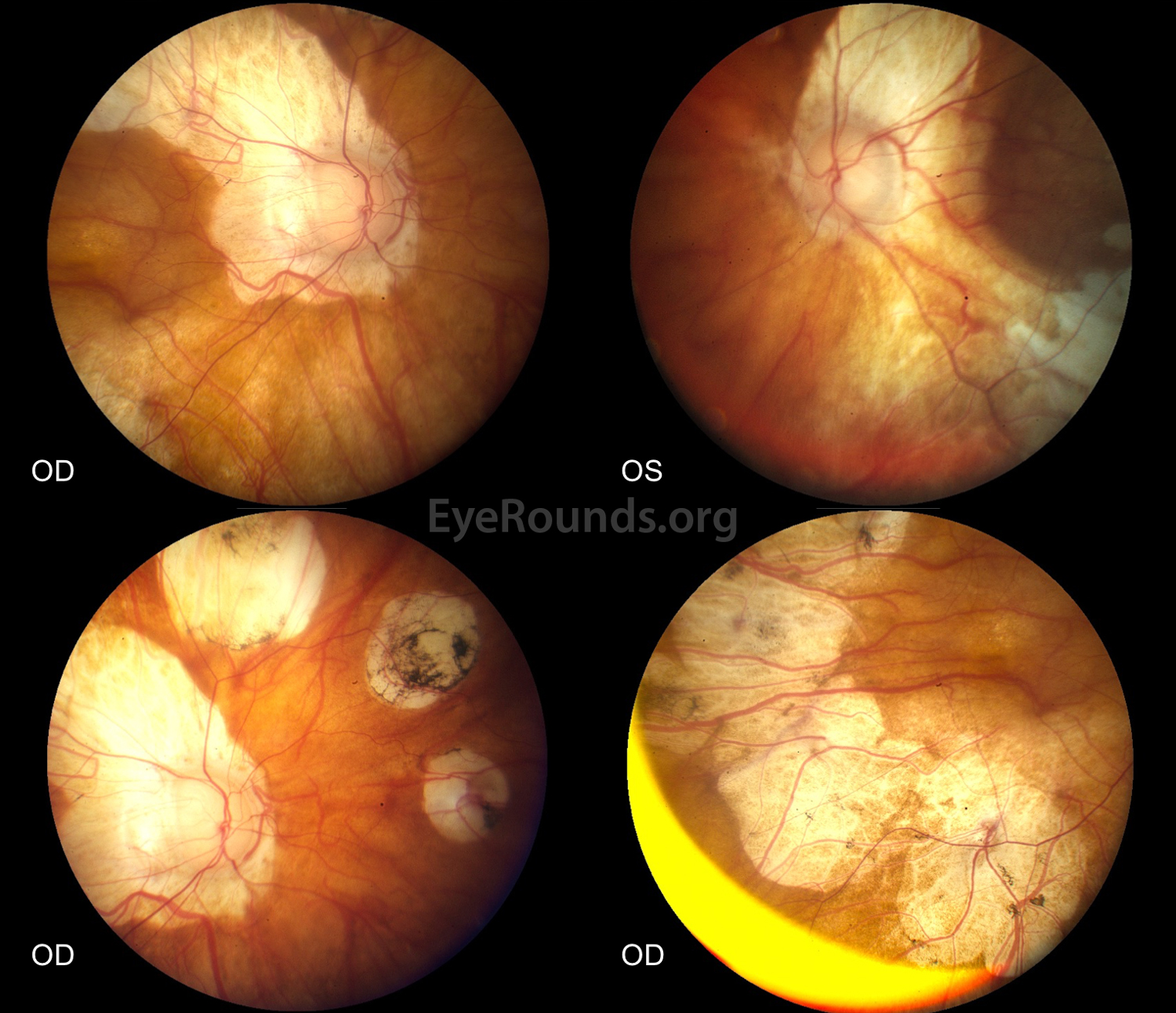
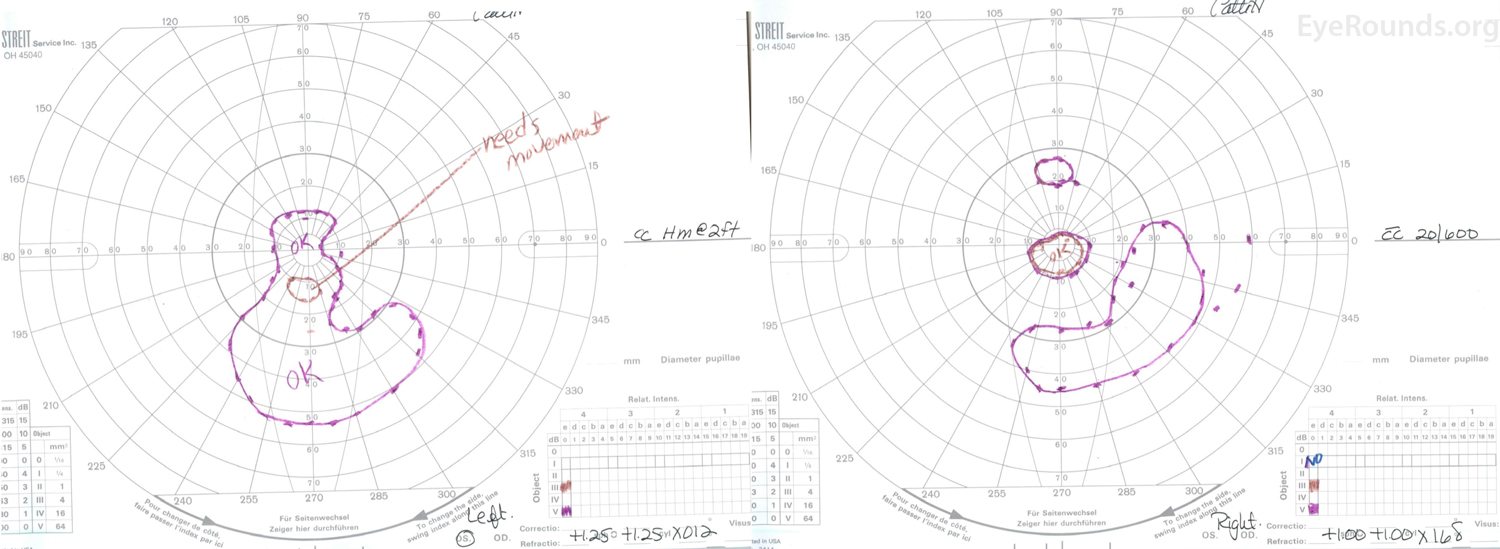
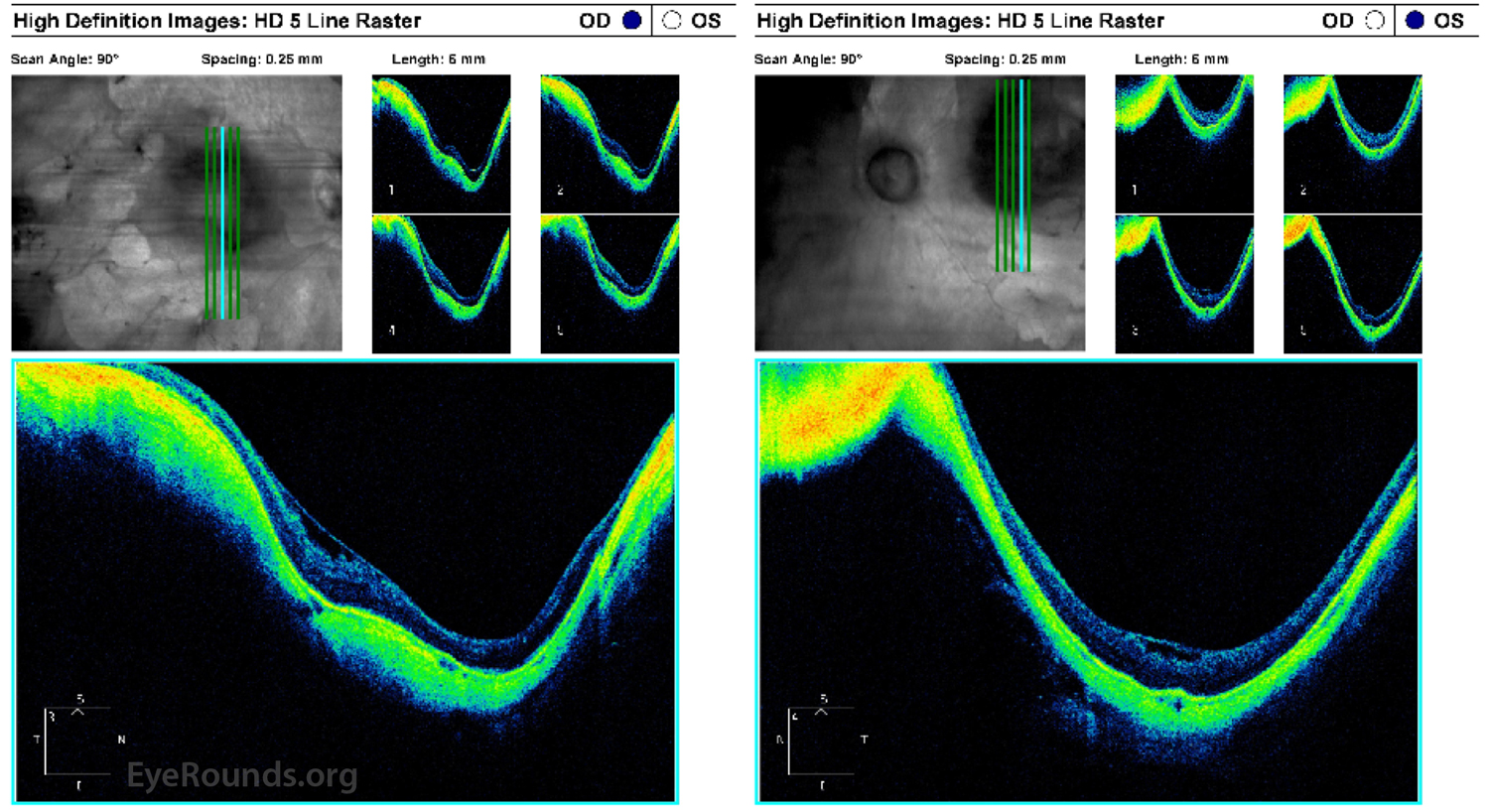
This patient had a lifelong history of profound hearing loss and vision loss in the left eye (OS) greater than right eye (OD) in the setting of Marshall syndrome with high myopia and aphakic glaucoma in both eyes (OU). She underwent strabismus surgery for esotropia as a child and bilateral extracapsular cataract extraction when she was 27-years-old. Her visual acuity progressively decreased to 20/600 OD and hand motions OS due to myopic degeneration OU. Dilated funduscopic examination showed numerous, scattered chorioretinal atrophic regions, vascular attenuation, and large posterior staphylomas OU (Figure 1). Goldmann visual fields showed a small, preserved central island of vision OU (Figure 2). Optical coherence tomography of the macula showed staphylomatous changes with severe retinal and choroidal thinning OU (Figure 3).
Marshall syndrome is a rare autosomal dominant syndrome that presents with pathologic myopia, congenital cataracts, sensorineural hearing loss, hypertelorism, and a flattened nasal bridge. Patients with Marshall syndrome have COL11A1 gene mutations leading to abnormalities in the production of collagen; mutations in this gene are also found in Type 2 Stickler's syndrome. Strabismus, retinal detachments, arthritis, and ectodermal abnormalities are common in Marshall syndrome [1].

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.