Chief Complaint: Left eyelid mass
History of Present Illness: A healthy 20-year-old female presented to the Oculoplastics Clinic with a 9-month history of left upper lid droopiness. Over the same period of time, she also noted a "bump" at the nasal aspect of her upper eyelid and felt that it was increasing in size. She denied any vision changes, ocular pain, pain with eye movement, or headaches. A complete review of systems was negative.
Past Ocular History: Myopia
Medical History: Non-contributory
Medications: None
Review of Systems: Negative
Visual acuity
Pupils: Briskly reactive without relative afferent pupillary defect
Extraocular Motility: Full OU
Intraocular pressure:
| Right | Left | |
|---|---|---|
| External | Normal | Fullness of superonasal orbit |
| Exophthalmometry | 17 mm | 18 mm |
| Palpebral Fissure | 10 mm | 9 mm |
| Margin Reflex Distance | 4 mm | 4 mm with medial ptosis |
| Palpation | Within normal limits | Superonasal immobile, hard, smooth lesion |
Slit lamp exam: Normal OU
Dilated fundus exam: Normal disc with 0.2 cup to disc ratio and normal macula, vessels and periphery OU
 |
|---|
 |
 |
 |
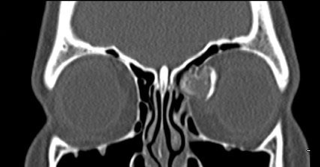
Given the history of recent growth, the decision was made to perform an excisional biopsy of the lesion. The patient was taken to the operating room, where an anterior orbitotomy via an upper lid crease incision was performed. The dissection was continued superiorly in the preseptal plane to the level of the orbital rim superonasally and continued further through the orbital septum. The tumor and its extent was identified (Figure 5). The lesion became freely mobile once the ethmoid sinus was entered. Dissection continued until the mass was free of its attachments and removed (Figure 6). Anatomic pathology demonstrated histopathologic findings consistent with an osteoid osteoma and no evidence of atypia. The patient had no post-operative complications and is doing well.
Primary orbital bone tumors constitute a very small percentage of all orbital tumors. More often, osteomas originate from the paranasal sinuses. Among the bony orbital tumors, fibrous dysplasias and osteomas are the most commonly encountered entities (Selva et al 2004).
An osteoid osteoma is a benign skeletal neoplasm of unknown etiology that is composed of osteoid and woven bones. Osteoid osteomas can occur in any bone, but in approximately two thirds of patients, the appendicular skeleton is involved. These lesions are encountered infrequently in the skull and facial bones, and they are usually smaller than 1.5 cm in diameter when they occur in these locations (Greenspan 1993). Osteomas are slow growing lesions that do not metastasize.
A review of systems is important to perform because if joints are involved, pain and swelling may be among the presenting symptoms. Skull-based osteomas are often completely asymptomatic, unless they arise in an area that compromises their vision or hearing. Often, these lesions are detected on imaging inadvertently during a workup for another reason (Benatiya Andaloussi et al 2006).
Osteoid osteomas generally occur in the frontal and ethmoid bones (Sires et al 1999). Radiographically, these tumors are well-circumscribed with dense cortical sclerosis surrounding a radiolucent nidus. Grossly, the lesion has a glistening, white to pink color and is either smooth or with rounded protuberances often described as being "knob-like." The interface between the osteoma and surrounding bone is usually abrupt.
Histopathologically, these lesions have a central nidus of loose fibrovascular tissue surrounded by irregular trabeculae of bone and osteoid (unmineralized, organic bone matrix prior to bone maturation). The amount of osseous (mineralized, mature bone) and osteoid tissue varies within the nidus and is reflected in its radiologic opacity.
| Benign | Malignant |
|---|---|
|
Osteoid osteoma Fibrous dysplasia Ossifying fibroma Osteoblastoma Chondroma Giant cell tumor |
Osteosarcoma Chondrosarcoma Mesenchymal chondrosarcoma Ewing sarcoma |
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Benatiya Andaloussi I, Touiza E, Bhallil S, et al. Orbital osteoma: three case reports. Bull Soc Belge Ophtalmol. 2006;(300):73-9.
Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma. Clinical, imaging, pathologic, and differential considerations. Skeletal Radiol. 1993;22(7):485-500.
Selva D, White VA, O'Connell JX, et al. Primary bone tumors of the orbit. Surv Ophthalmol. 2004;49(3):328-42.
Sires BS, Benda PM, Stanley RB Jr, et al. Orbital osteoid osteoma. Arch Ophthalmol. 1999;117(3):414-5.
Suggested Citation Format: Rogers GM, Carter KD. Orbital Osteoma. EyeRounds.org. June 3, 2011; Available from: https://eyerounds.org/cases/133-orbital-osteoma.htm
Graff JM, Oetting TA, Kwon YH. Intralenticular Foreign Body : 23-year-old male with staple in the eye. EyeRounds.org. January 31, 2007 ; Available from: http://www.EyeRounds.org/cases/63-Intralenticular-Foreign-Body-Open-Globe.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.