Chief Complaint: 35-year-old female complaining of blurred vision and flashing lights in the right eye.
History of Present Illness: 35-year-old female presented to her local ophthalmologist complaining of blurred vision, flashing lights and intermittent floaters in the right eye for the past week.
Past Ocular History: While pregnant 13 years ago she had two episodes of loss of vision in the left eye. They lasted 30 to 40 minutes and resolved on their own. She was diagnosed with migraine with aura.
Medical History: Cutaneous melanoma excised at age 5; it began as a large birthmark that later changed color. She also suffers from eczema.
Medications: Daily multivitamin.
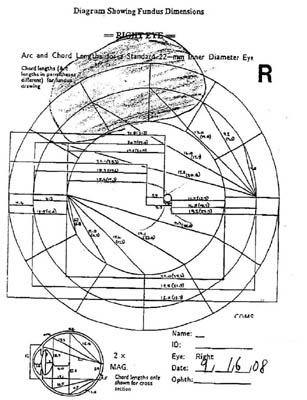 |
Clinical Course: This mass was diagnosed clinically as a cilio-choroidal melanoma with localized retinal detachment. Chest and abdominal CT were performed and were normal. Liver function tests were also normal. After extensive discussion of potential treatment options, the patient elected for enucleation of the right eye.
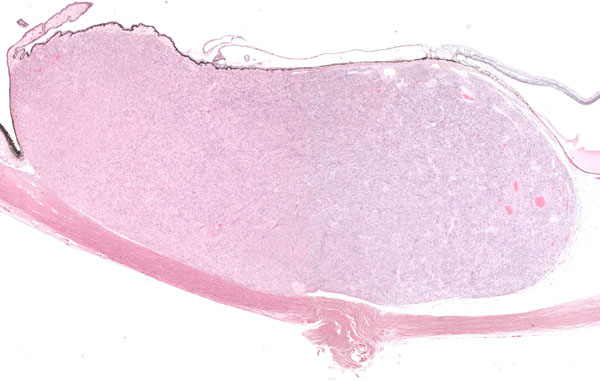
Gross Pathology: The enucleated globe was received at the F.C. Blodi Eye Pathology Laboratory. The globe was sectioned and an elevated mass was noted at the ciliary body. (See Figure 2) Upon sectioning, the tumor was cream colored and dome-shaped. (See Figure 3)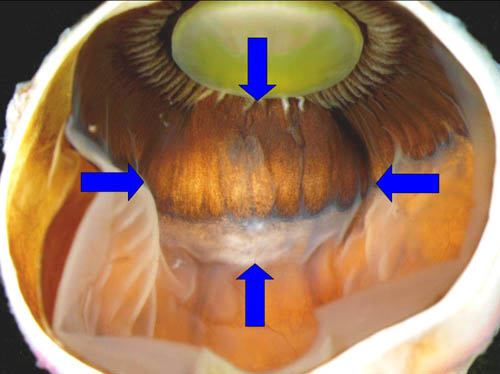 |
 |
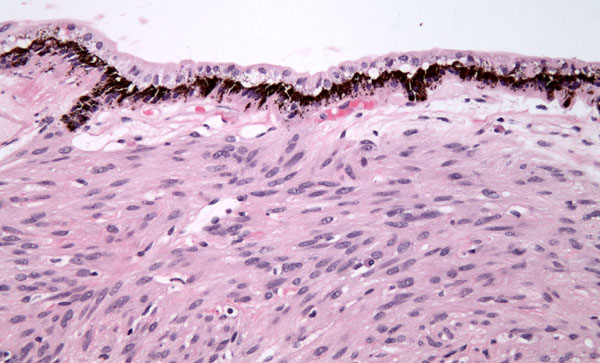
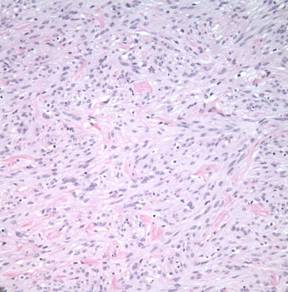
Histopathology: Microscopic examination revealed that the overlying basement membrane of the pigment epithelium was largely intact, there was no scleral invasion, and a small exudative retinal detachment was present posterior to the tumor. The neurosensory retina, optic nerve and uninvolved choroid were unremarkable. (Figures 4 and 5)
 |
|
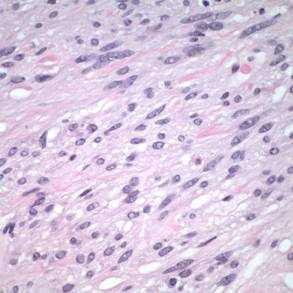
At higher power, fascicular bundles of spindle cells with occasional intervening bundles of collagen were noted. Cell nuclei demonstrated a vesicular chromatin pattern with occasional indistinct nucleoli and cytoplasm devoid of pigment. No mitoses were present in 40 high-power fields. Scattered lymphocytes were present. No necrosis was seen. (See Figure 6)
| 6A. Hematoxylin-Eosin Stain, 50x | 6B. Hematoxylin-Eosin Stain, 300x |
 |
 |
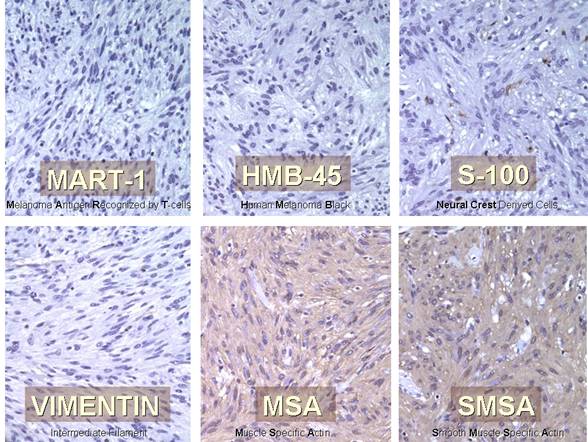
A standard immunohistochemical panel was performed to better determine the cell of origin of this tumor. MART-1 and HMB-45, markers for cells of melanocytic origin, were negative in tumor cells. S100, a marker for cells of neural crest origin, was negative. Vimentin, a marker for cells of epithelial origin, was also negative. Muscle specific actin (MSA) and smooth muscle specific actin (SMSA) were both diffusely positive in tumor cells (figure 7).
 |
Ciliary body leiomyoma is a benign smooth muscle neoplasm, usually found in the ciliary body and anterior choroid (iris lesions reported). It has a strong predilection for young women.
The pathogenesis is unclear. Two hypotheses propose different tumor origins. The first one suggests that the tumor is derived from the smooth muscle layer of vessel walls, while the second one proposes the ciliary muscle itself as the tumor origin.
The old criteria for histopathological diagnosis have become less applicable with the wide use of diagnostic immunohistochemistry. Electron microscopy may also be used, but immunohistochemistry is easier to obtain, less costly and more reliable in paraffin-embedded tissue.
It is always important to exclude a leiomyosarcoma. The major differences between the two tumors are the absence of intra- or extraocular extension and the low mitotic rate of leiomyoma on histopathology.
The clinical diagnosis of ciliary body leiomyoma is often challenging. Several clinical tests have been used in an attempt to diagnose leiomyoma. Ultrasound shows a well-defined, homogeneous lesion with wide variation in internal reflectivity and orbital shadowing behind the mass. Unfortunately these findings are not consistent or conclusive. MRI has also been used but it only shows an intraocular mass that is isointense to brain, and is of little utility in diagnosis.
Even though a leiomyoma is a benign tumor, complications may arise from local damage caused by its growth. These complications include subluxation of the lens, glaucoma and retinal detachment.
Partial lamellar sclero-uvectomy and transscleral resection have been performed with excellent results and sparing of the eye. In some cases, the large size of the mass leaves no choice other than enucleation. The prognosis after resection of the tumor is excellent as there are no reported recurrences.
Even though rare, leiomyoma should be considered in the differential diagnosis of amelanotic uveal tumors, especially in young females and/or if it lacks typical melanoma features.
| Leiomyoma | Melanoma |
|---|---|
Female predilection |
Slight predilection for males |
12–55 years, mean 30 years |
Mean 55 years |
Transmits light readily and can even reflect light |
Relative shadow |
Affects ciliary body, rarely purely in the choroid |
Frequently purely in the posterior choroid |
Supraciliary or suprachoroidal space |
Arises from the uveal stroma |
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Fernandez de Castro JP, Syed NA. Clinicopathologic Correlation: Ciliary Body Leiomyoma. EyeRounds.org. Sept. 9, 2009; Available from: http://www.EyeRounds.org/cases/64-Leioma-Clinicopathologic.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.