Chief Complaint:14-year-old male with "poor vision since birth"
History of Present Illness: An otherwise healthy 14-year-old boy presented for a second opinion regarding optic nerve hypoplasia. He was diagnosed with congenital nystagmus after presenting with "difficulty tracking" and was noted to have optic nerve hypoplasia in both eyes. The patient was otherwise completely healthy and had done well over the years with low vision services including a closed circuit television and magnifiers at home. His vision had remained stable and he had no new visual complaints.
The parents had researched their son's condition and were considering traveling to China for "stem cell transplantation" to treat their son's optic nerve hypoplasia. They came to The University of Iowa Hospitals and Clinics to establish care with a U.S. Ophthalmologist who could perform the required pre-op exam and post-op follow up examinations. They brought a large amount of online information about stem cell therapy and its promising results.
Past Ocular History: Optic nerve hypoplasia OU, congenital nystagmus
Medical History: Normal growth and development. No hospitalizations or surgeries.
Medications: None
Family History: Diabetes and hypertension
Social History: No tobacco or alcohol use.
 |
 |
 |
 |
Course: The neuro-ophthalmologist at UIHC talked at length with the family. He explained to them that intravenous and intrathecal delivery of stem cells has not yet been proven to be an effective treatment for optic neuropathies including optic nerve hypoplasia. He discussed the biologic rationale for stem cell transplantation and the potential risks of the procedure. He tried to explain to the family the differences in regulation and scientific scrutiny of these procedures in the US compared with China. In addition, he explained that at this time "we cannot ensure that the neuronal connections will be made even if the implanted stem cells made it to the target organ." An extensive discussion followed including the emerging research on stem cells and its successful application in other fields. The conclusion of the consulting neuro-ophthalmologist was that "at the present time that stem cell transplantation was not a proven effective or safe procedure for optic nerve hypoplasia." He concluded that the risks involved outweigh any benefit. He recommended waiting until the procedure had passed through significant safety and efficacy human trials before subjecting their child to the procedure.
The neuro-ophthalmologist was very supportive of the family, and offered to go through the online information with them in detail. The parents felt disappointed by the news, however, and were frustrated that their appointment did not support their own investigations on the internet.
This case highlights a number of professional and ethical considerations with respect to patient advocacy and the scientific process.
Dissatisfaction with traditional medicine, or with an insufficient "cure" for optic nerve hypoplasia, has led some parents to seek alternative sources of care. News stories have reported parents flying their children to mainland China for umbilical cord stem cell (CSC) infusions. CSCs are extracted from the umbilical cords of Chinese mothers and their newborns and injected into the fluid around the spinal cord of the patient. The parents are led to believe by Chinese doctors that CSC infusions are an effective treatment for optic nerve hypoplasia (ONH). The cost of these treatments, paid for entirely out-of-pocket by the parents, can be $50,000 or more.
For many alternative therapies, the "proof" of efficacy exists online, in advertising sections, or in homeopathic health journals. The studies are often done without control subjects or objective endpoints. In many cases, the cited evidence consists of single case reports and patient testimonials. Patients often expect their physicians to understand and comment on these complementary therapies. For these reasons, alternative therapies create unique ethical circumstances that cannot be ignored by the practicing ophthalmologist.
In this particular example, the patient has had very poor vision since birth. Evidence-based Western medicine has little to offer him at this point in time other than low vision aids to maximize the vision that he does have. His parents were understandably drawn to the promises of visual improvement with an alternative treatment. Ideally, the physician will validate the patient's or family's desire to explore all therapeutic possibilities, but will also give his or her clinical opinion about the patient's best interests. This form of advocacy requires a combination of compassion, empathy, and knowledge of both conventional and alternative therapies.
This case highlights the physician's obligation to produce and promote honest science.
The fundamental ethical issue in promoting new treatments is the obligation to fulfill the requirements of evidence-based medicine. The public assumes that persons with an "MD" behind their names are committed to the scientific process in which treatments are validated. According to the Belmont Report, "When a clinician departs in a significant way from standard or accepted practice, the innovation does not, in and of itself, constitute research."
Another ethical issue associated with alternative therapies relates to communication. On concluding an investigation of an alternative therapy, the ophthalmologist bears an ethical responsibility to report the data and results using the appropriate avenues of communication. Rather than contacting the public media first with promising preliminary results, the more correct and responsible approach is to present the information at recognized meetings of peers, or to publish the results in a scientific journal refereed by other knowledgeable physicians in the field. By following the peer review process, the ophthalmologist protects the public from the misuse of a new therapy. The promulgation of flawed data and conclusions or of promised benefits where there are none must be avoided.
Any alternative therapy offered to the patient should have a high likelihood of benefiting the patient, and the remuneration for that treatment should be reasonable and commensurate with similar treatments. To reap undue financial profit from the use of non-validated complementary therapies is unethical.
It is the responsibility of the ophthalmologists to uphold the trust placed in them by patients, and to offer or recommend only those procedures that are in the patients' best interests.
Optic nerve hypoplasia is a variable condition that may be unilateral or bilateral, associated with good or poor visual function, and may occur in association with other ocular or neurologic findings. Although once considered a rare finding, it is now the most common congenital optic disc anomaly encountered in pediatric ophthalmic practice and a common cause of congenital blindness.
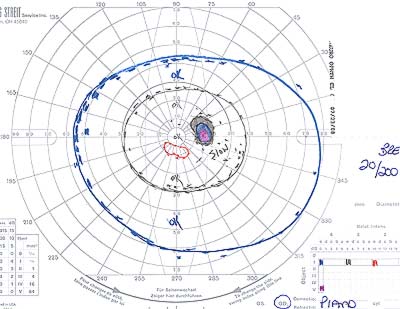
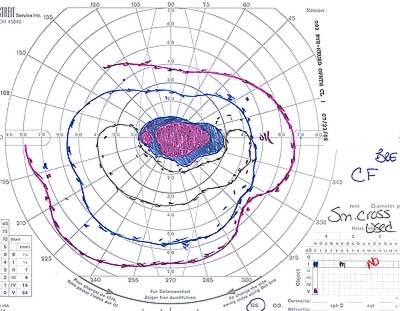
The visual acuity ranges from normal with only minimal visual field defects to no light perception. The visual field defects are typical for optic nerve damage. Peripheral and arcuate defects are common (See Figures 1 and 2).
The prevalence of bilateralism is 56-92%. If the condition is unilateral, a relative afferent pupillary defect may be detected. Other dysfunctions of the afferent system that may be detected include color vision, red desaturation and brightness perception.
On ophthalmoscopy, the optic disc appears smaller than normal (usually one half to one third of normal), although this finding may be subtle. The comparison of horizontal disc diameter to the disc-macula distance may aid in detection. The disc may be pale or gray. The retinal vessels may appear large relative to the small disc, and the vessels may be tortuous. At times, the hypoplastic disc is surrounded by a ring of sclera and a ring of hyperpigmentation: the "double ring sign".
Although the exact mechanism of optic nerve head hypoplasia is not completely understood, it is believed to represent a dysplasia of the retinal ganglion cell layer with an associated loss of the nerve fiber layer, secondary to some interruption in fetal development. Underdevelopment of the optic nerve results and the posterior scleral foramen "fills in" with connective and scleral tissues.
Many disorders have been implicated in this disorder, including gestational diabetes, maternal infection by cytomegalovirus, syphilis, rubella, fetal alcohol syndrome and other drug use by the mother while pregnant. Either unilateral or bilateral optic nerve hypoplasia may be associated with midline or hemispheric brain defects, endocrinologic abnormalities and congenital suprasellar tumors (rarely). Optic nerve hypoplasia may be part of larger clinical syndromes such as Septo-optic dysplasia, de Morsier syndrome which consists of optic nerve hypoplasia, pituitary dwarfness, and an absent septum pellucidum. The corpus callosum may be thinned or absent.
Optic nerve hypoplasia is a congenital condition. Appropriate management begins with proper diagnosis. Visual field testing can be used to confirm suspicions based on clinical exam.
In addition, photography of the posterior pole of the affected eye allows measurement of the disc-macula/disc-disc (DM/DD) ratio. This allows comparison of the horizontal diameter of the nerve head to the distance between the fovea and the center of the nerve. In a normal eye, the DM/DD measures between 2:1 and 3.2:1. Ratios greater than this suggest hypoplasia.
An MRI scan is recommended in all cases of optic nerve hypoplasia, and endocrine consultation should be considered based on history and MRI findings.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
see related: Case 10: Optic Nerve Hypoplasia
Pham L, Lee AG. Communicating with patients about Alternative Therapies: A case of optic nerve hypoplasia. EyeRounds.org. November 12, 2008; Available from: http://www.EyeRounds.org/cases/88-Professionalism-Alternative-Therapies.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.