Chief Complaint: 7 month old boy who became unresponsive while feeding.
History of Present Illness: According to the child's parent, he was being fed when he began choking. Shortly thereafter, he went limp and became unresponsive. CPR was started and 911 was called. Paramedics found the patient to be apneic and pulseless. Pupils were fixed and dilated. CPR was continued and the patient was intubated en route to the hospital.
Upon arrival at the hospital, an arterial blood gas was obtained, which showed the child to be severely acidotic (ph 7.02). Non-contrast head CT revealed subdural hemorrhage and cerebral edema. An intracranial pressure monitor was placed, and the patient was admitted to the pediatric intensive care unit. The child was noted to have bilateral swelling of his upper extremities and scattered bruises.
Hypertonic saline infusion was started due to elevated intracranial pressures and Dilantin was administered due to seizure activity noted on arrival.
At this point, due to suspicion for nonaccidental trauma, a hair sample was obtained for illicit drug testing and blood was sent for a complete blood count (CBC), platelet function analysis (PFA), von Willebrand panel, prothrombin time (PT), international normalized ratio (INR), partial thromboplastin time (PTT), and liver function tests (LFT's). Skeletal survey x-rays were ordered according to University of Iowa's child abuse protocol. The hospital's child abuse pediatrician and pediatric ophthalmology were consulted.
Past Ocular History: None.
Medical History: The patient was reportedly healthy prior to the incident. He was the product of an uncomplicated twin gestation and had a healthy twin sibling. The twins were born at term via spontaneous vaginal delivery.
Medications: None.
Family History: Noncontributory.
Social History: The patient lived with his parents and two siblings.
 |
 |
 |
 |
| Figure 3a: Left humerus fracture | Figure 3b: Multiple rib fractures. |
|---|
Hospital Course: Despite infusion of hypertonic saline, the patient's intracranial pressure remained significantly elevated. Following administration of fresh frozen plasma and platelets, his PT, INR, PTT, and fibrinogen normalized and remained within normal limits. On the fourth day of hospitalization there was evidence of brain herniation. A diagnosis of brain death was made by the pediatric neurology service and the patient was pronounced legally dead. Prior to withdrawal of treatment, his organs were harvested for transplantation.
The Department of Human Services had removed his siblings from their home and placed them in protective custody. They also showed signs of abuse. The patient's father was arrested for suspicion of abuse.
Eye
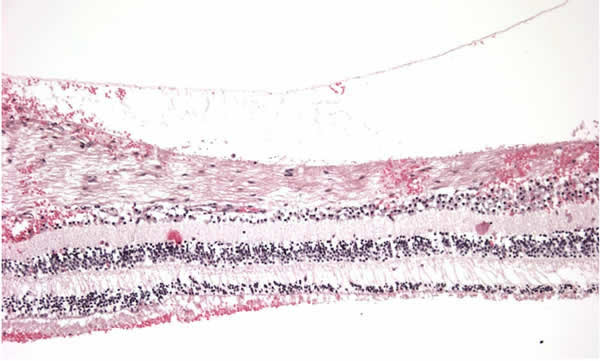
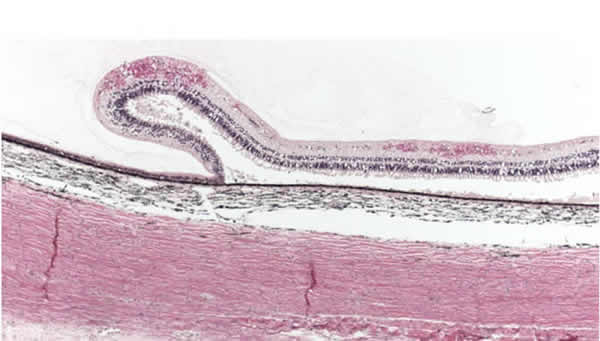
| Figure 4a: Optic sheath extradural and subdural hemorrhage |  |
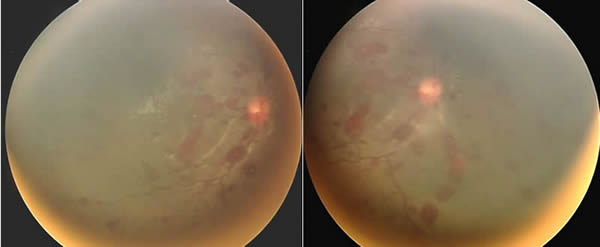
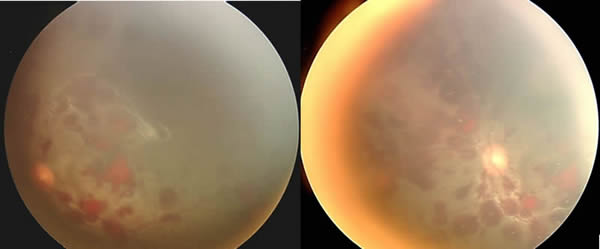
 Figure 4b: Diffuse retinal hemorrhages and several preretinal hemorrhages OD. |
 Figure 4c: Diffuse retinal hemorrhages and macular preretinal hemorrhage OS. |
 |
|---|
 |
|---|
 |
|---|
Discussion: Every year in the United States, hundreds of thousands of children are the victims of abuse or neglect. In 2005, it was estimated that 1,460 fatalities resulted from this abuse. Non-accidental trauma (formerly known as Shaken Baby Syndrome) is an important type of child abuse that affects 1200-1400 children every year. Non-accidental trauma is of major concern to physicians and child abuse specialists because it is associated with a mortality rate of approximately 30%. Of those that survive the trauma, many, if not most, are left with significant long-term disabilities including: blindness, cerebral palsy, mental retardation, and seizure disorder.
Non-accidental trauma is most likely to result from abuse by a male caregiver. Fathers and boyfriends make up about 75% of abusers. Aside from being male, perpetrators are more likely to be young parents, have a lower educational level, have a history of substance abuse, and have a prior history of domestic violence. Certain characteristics of the infant also make them more likely to be abused. These include: age under 6 months, male sex, frequent crying, premature or low birth rate, or having special needs and disabilities.
Non-accidental trauma may be initially misdiagnosed by healthcare providers because signs and symptoms may be nonspecific. Poor feeding, vomiting, apnea, irritability, seizures, decreased tone, and decreased consciousness are just a few of the ways that non-accidental trauma may present. Diagnosis is also complicated due to frequent attempts by caregivers to conceal the true etiology of the patient's injuries; the physician is often given a vague or inconsistent account of the events surrounding the child's injuries. When given a vague history, or given a history that seems inconsistent with the extent of the child's injuries, a care giver should suspect abuse.
It is important to note that the diagnosis of non-accidental trauma cannot be made based upon isolated exam findings. It is a diagnosis that requires the synthesis of information from the physical exam, radiologic studies, ophthalmic exam, and laboratory studies. Often, the severity of the injuries is out of proportion to the history as given by the caregiver. After obtaining a careful history, the practitioner should perform a thorough physical exam paying close attention to the child's level of consciousness, tone, and movements. Skin abnormalities and soft tissue swelling are also important look for. Blood should be sent for a CBC, liver function tests, amylase, and coagulation studies including PT, PTT, INR, PFA, and von Willebrand factor. If non-accidental is suspected, skeletal survey x-rays and a non-contrast head CT should be obtained. X-ray findings such as multiple fractures of various ages, spiral fractures of long bones, skull fractures, and multiple rib fractures are especially suggestive of abuse. Subdural hematoma is the most common finding on head CT, but other findings such as cerebral edema, subarachnoid hemorrhage, and vascular infarction are also consistent with inflicted trauma.
Finally, the evaluation of non-accidental trauma should include the consultation of an ophthalmologist, and a dilated fundus exam if possible. A detailed ophthalmic note should be generated with photographic documentation of the retinal findings when possible. This is because retinal hemorrhage is both a sensitive and specific finding. Retinal hemorrhage is the most common ocular finding in non-accidental trauma, and can be found in approximately 80% of cases. Hemorrhages often consist of concomitant intraretinal, preretinal, and vitreous hemorrhage. While the majority of these hemorrhages will be found at the posterior pole, hemorrhages that extend all the way to the ora serrata are especially suggestive of abuse. Hemorrhages in non-accidental trauma tend to be bilateral and are predictive of both poor visual and neurologic outcomes. It should be noted that there are a number of conditions that have been associated with retinal hemorrhages in infants (see table 1). However, extensive bilateral retinal hemorrhages involving multiple layers of the retina, and extending into the far periphery are rarely seen in other conditions, even severe accidental injuries.
|
Other findings associated with non-accidental trauma included circumferential macular folds, and retinoschisis. It is believed that both of these findings result from tractional forces exerted on the retina due to the firm adhesion of the vitreous face to the internal limiting membrane in young eyes. Circumferential macular folds are a poor prognostic indicator, and are associated with a mortality rate that exceeds 50%.
While not visible on premortem examination, optic nerve sheath hemorrhage is a common finding during autopsy in cases of non-accidental trauma. Like intracranial bleeding, optic nerve sheath is most commonly found in the subdural space. However, intradural, subarachnoid, and epidural hemorrhages extending into the surrounding fat and extraocular muscles may also be found. Another finding not seen clinically but that is highly suggestive of non-accidental injury is the presence of peripapillary intrascleral hemorrhage.
The ophthalmic examination provides important information not only regarding visual morbidity, but regarding overall mortality as well. The presence and severity of retinal hemorrhages, presence of circumferential macular folds, and absence of pupillary and visual response have all been shown to be predictors of mortality. Thus, visual and neurologic outcomes are closely linked in non-accidental trauma. Up to 50% of children that survive non-accidental trauma will be left with some level of visual impairment. Visual impairment may result from occipital cortical damage, optic atrophy, retinal scarring, and amblyopia induced by nonclearing vitreous hemorrhage.
In summary, non-accidental trauma in infants is an all-too-commonly encountered phenomenon, which can present with non-specific findings. No one finding, whether ophthalmic or otherwise, is diagnostic for non-accidental trauma. The diagnosis requires the synthesis of laboratory, radiologic, ophthalmic, and other clinical information.
Diagnosis: Non-accidental trauma (commonly known as Shaken Baby Syndrome)
EPIDEMIOLOGY
|
SIGNS
|
DIAGNOSIS
|
TREATMENT
|
Wendel LJA, Longmuir SQ, Syed NA. Non-accidental Trauma: An unresponsive infant with bilateral retinal hemorrhages. EyeRounds.org. February 12, 2009; Available from: http://www.eyerounds.org/cases/92-nonaccidental-trauma.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.