
Rosacea, sometimes referred to as acne rosacea, is a chronic dermatologic condition characterized by sebaceous gland dysfunction of the face, neck, and shoulders. Patients may experience vasomotor lability and facial flushing with consumption of alcohol, hot beverages, spicy foods, or other substances. Rhinophyma is a characteristic sign, but may not be present until late in the disease. Ocular manifestations are present in 50% of cases. They include recalcitrant blepharitis, meibomian gland dysfunction, telangiectasia of the eyelid margin, and recurrent chalazia. Longstanding ocular surface inflammation can result in chronic conjunctivitis, episcleritis, iridocyclitis, keratitis, marginal corneal infiltrates, or corneal ulceration. The keratitis associated with rosacea is most commonly inferior, presumably due to the accumulation of inflammatory cytokines in the tear film above the lower lid. It results in the formation of broad, "spade-shaped" pannus with vessels extending into gray or white peripheral stroma, occasionally with subepithelial infiltrates at the leading edge. Findings are usually bilateral, but may be asymmetric.
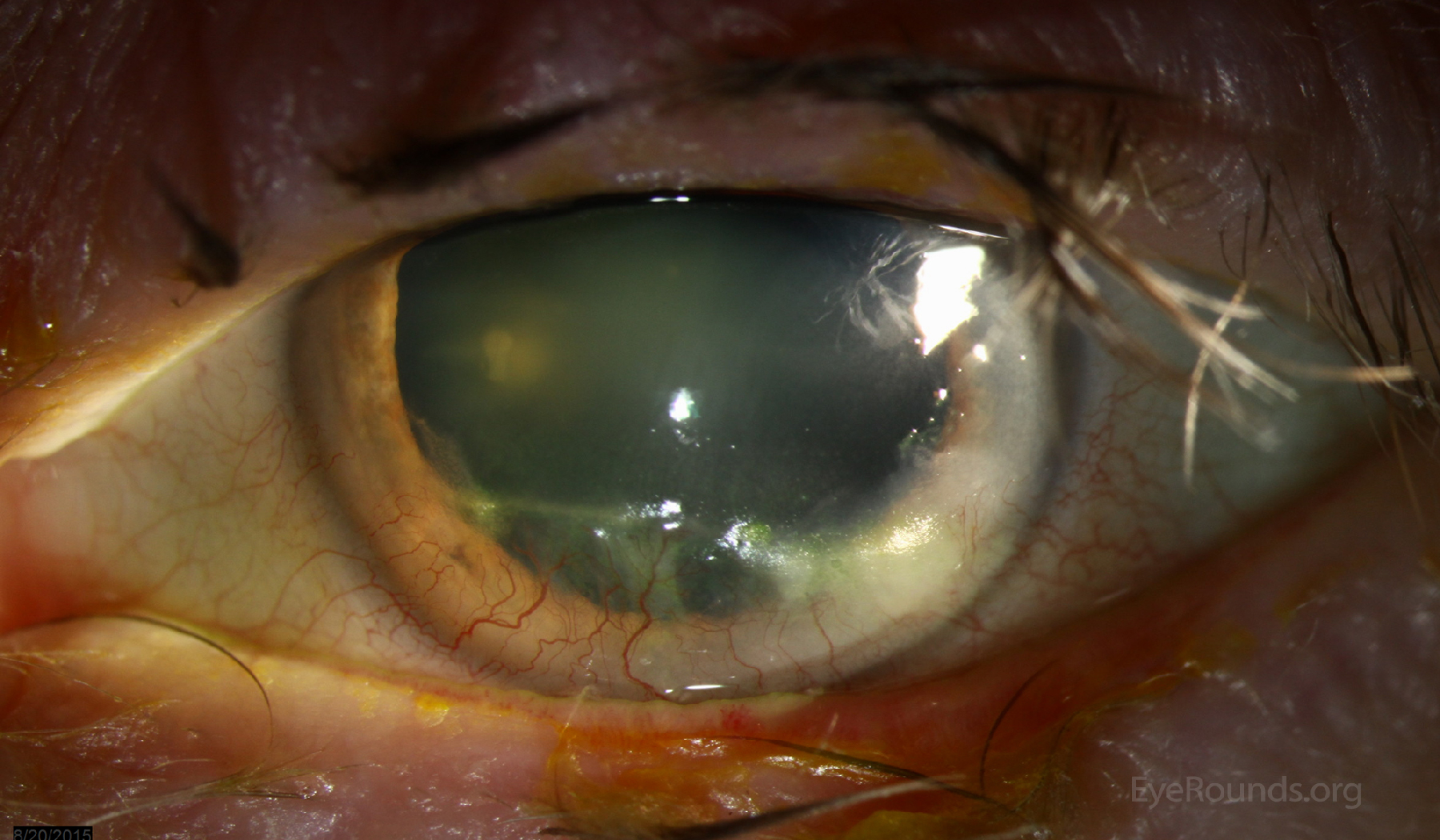
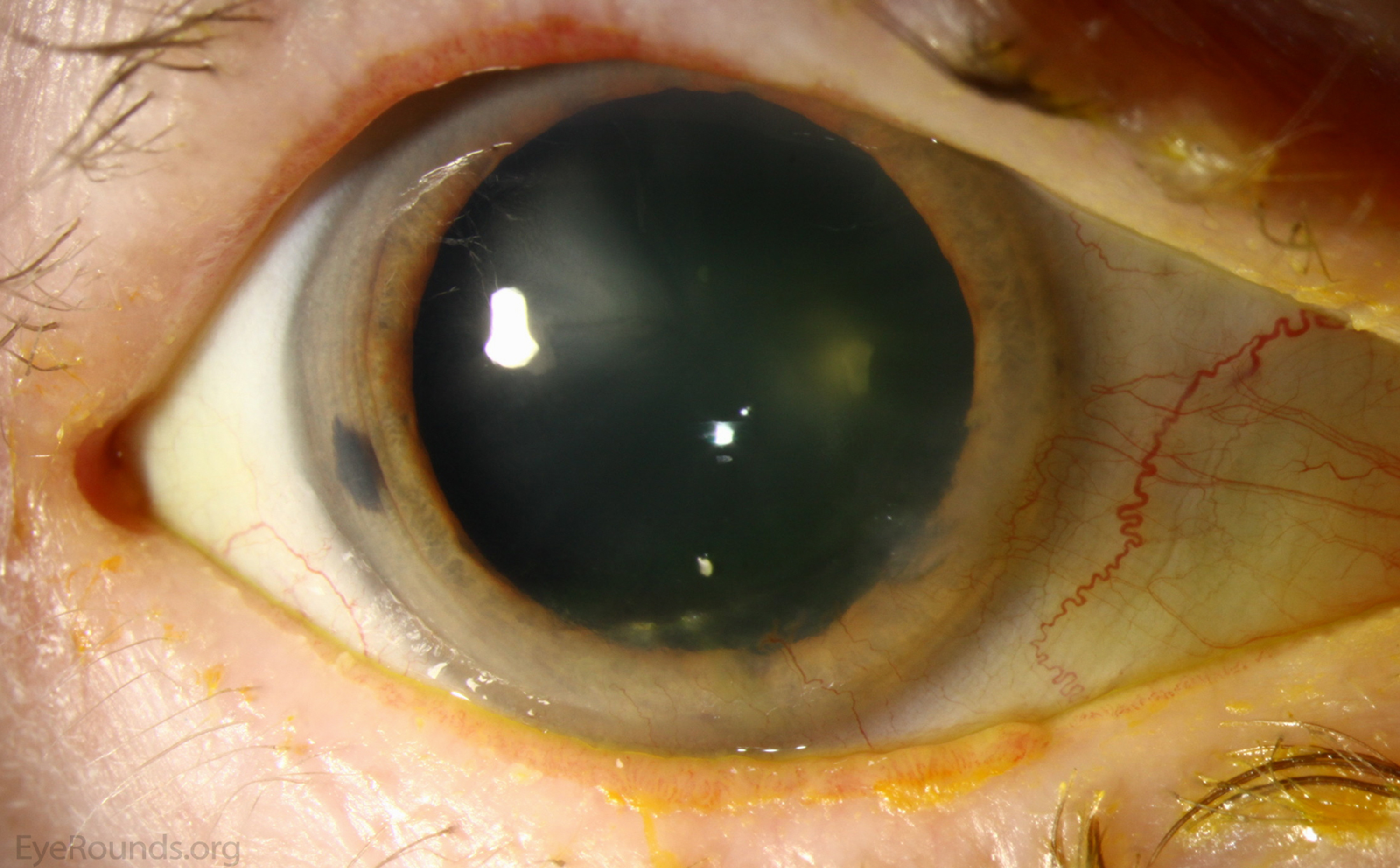

This 60-year-old male was referred due to progressive peripheral corneal ulceration. He was noted to have an inferior peripheral corneal epithelial defect with 70% underlying stromal thinning. There was a sterile-appearing infiltrate surrounding the ulcer and peripheral corneal neovascularization. He was also noted to have marked eyelid margin inflammation and telangiectasias, meibomian gland inspissation, and facial erythema and telangiectasias, consistent with ocular and facial rosacea. He was treated with oral doxycycline, oral fish oil supplements, warm compresses, preservative-free artificial tears every two hours, and a topical fluroquinolone four times daily. His epithelial defect healed and the area scarred without further progression.


Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.