Chief Complaint: 34-year-old female awoke with painless loss of vision OS 3 weeks prior to presentation.
History of Present Illness: She saw her local ophthalmologist immediately after the onset of vision loss. Her ophthalmologist noted 1+ vitreous cells, VF defect OS, and a head MRI was reported normal. A diagnosis of retrobulbar optic neuritis was made. Her vision continued to decline. One week prior to our evaluation, she complained of photopsias x 1 week and a diffuse, frontal headache x 3 days.
PMH/FH/POH: Previously healthy without prior ocular surgeries or trauma. She is 5'7" and weighs 250 lbs.
EXAM| OS | OD |
 |
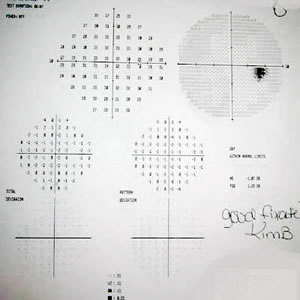 |
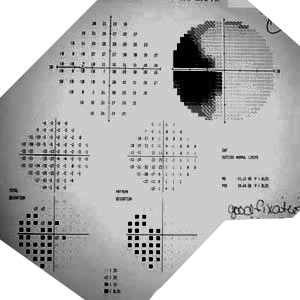
| Enlarge blind spot with superior and inferior visual field (VF) loss. The VF loss does not respect the vertical midline; thus, this lesion is unlikely to be cortical. | Full VF OD. |
| OS | OD |
|
|
| Extensive superior & inferior VF loss around where the blind spot should be located. The VF loss does not respect the vertical midline. Constriction of I2e (red), I4e (blue), I3e (grey), and V4e (purple) isopters. | Full VF. |
| OD | OS |
| Normal optic nerve and macula. | Incidental melanocytoma and peripapillary choroidal nevus. No optic nerve edema. Macula normal. |
| OD | OS |
|
|
|
| OD Waveform
|
OS Waveform
|
| Normal MERG OD. | Marked depression of retinal function OS. |
Our patient presented with: a normal optic nerve (except for the incidental finding of melanocytoma OS), normal dilated fundus exam, mild vitreous cells, decreased vision OS associated with RAPD, photopsias, headache, VF loss, and depression of retinal function OS illustrated by the MERG. Considering a normal MRI, age of the patient, and heavy stature of the patient, we felt that the patient may have presented as an atypical pseudotumor cerebri. Without disc swelling, the diagnosis of pseudotumor cerebri is not typical. The patient had a spinal tap which demonstrated a normal opening pressure.
The other symptoms and clinical presentation in this patient is more typical for acute idiopathic blind spot enlargement (AIBSE) syndrome or acute zonal occult outer retinopathy (AZOOR). This led us to perform a MERG which demonstrated depression of retinal function OS and confirmed the diagnosis of AIBSE/AZOOR. Some will call this disease AIBSE but others will call it AZOOR when there are large areas of retina involved. Several clinicians believe that AIBSE and AZOOR fall in the spectrum of the white dot syndromes, which are idiopathic chorioretinal inflammatory diseases. Some have suggested that AIBSE and AZOOR are multiple evanescent white dot syndrome (MEWDS) without the dots. AIBSE and AZOOR are less aggressive than the other white dot syndromes, and many patients with AIBSE/AZOOR will recover vision.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Doan A, Lee AG, Boldt HC: Acute Zonal Occult Outer Retinopathy (AZOOR) and Acute Idiopathic Blind Spot Enlargement Syndrome (AIBSE): 34-year-old female awoke with painless loss of vision OS 3 weeks prior to presentation. February 21, 2005; Available from: http://www.EyeRounds.org/cases/case18.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.