Idiopathic Intracranial Hypertension
(Pseudotumor Cerebri)
Michael Wall, M.D.
The University of Iowa
Department of Neurology and
Department of Ophthalmology and Visual Sciences
How is IIH treated?
Treatment for patient with IIH can be divided into medical treatment and surgical treatment. The cornerstone of medical treatment is weight loss. It does not appear to be the total number of pounds lost. Some patients are effectively treated by losing one pound every week or two for several months and then maintaining the weight loss. It has been shown that loss of 5-10% of body weight is often sufficient for optic disc edema to regress, symptoms resolve and vision improve.
Loss of fluid can also be obtained using diuretics (fluid pills). Diamox (acetazolamide) is the most commonly used medication. It is relatively safe but nearly all patients have tingling of the fingers and toes. This tingling is a benign symptom and suggests the medication is working. Patients also experience that carbonated soft drinks taste metallic. Less commonly, kidney stones can occur and rarely other blood disorders. Another diuretic commonly used that appears to be effective in some patients is Lasix (furosemide). More about Diamox.
While there is no evidence based treatment to guide medical therepy there is currently an ongoing National Eye Institute sponsored trial, the Idiopathic Intracranial Hypertension Treatment Trial. The trial has two aims. One is to determine if acetazolamide (Diamox) with a low sodium weight reduction diet is superior to placebo with the diet. The second aim is to investigate the cause of idopathic intracranial hypertension. Further information can be found at the NORDIC website .
The surgical treatments currently used are optic nerve sheath fenestration (making slits in the optic nerve sheath or covering) (Figure 11) and CSF shunting procedures (running a tube from the spinal fluid space into the abdominal cavity or a vein). These procedures are used when patients do not respond adequately to medical therapy. Optic nerve sheath fenestration is done first by an incision into the orbit. The eyeball is moved to the side and the optic nerve sheath is exposed. Slits or a large hole are then placed in the optic nerve sheath and fluid drains out, thereby taking pressure off the optic nerve.

from Sergott RC, Savino PJ, Bosley TM. Modified optic nerve sheath decompression provides long-term visual improvement for pseudotumor cerebri. Arch Ophthalmol 1988; 106:1391-1397.
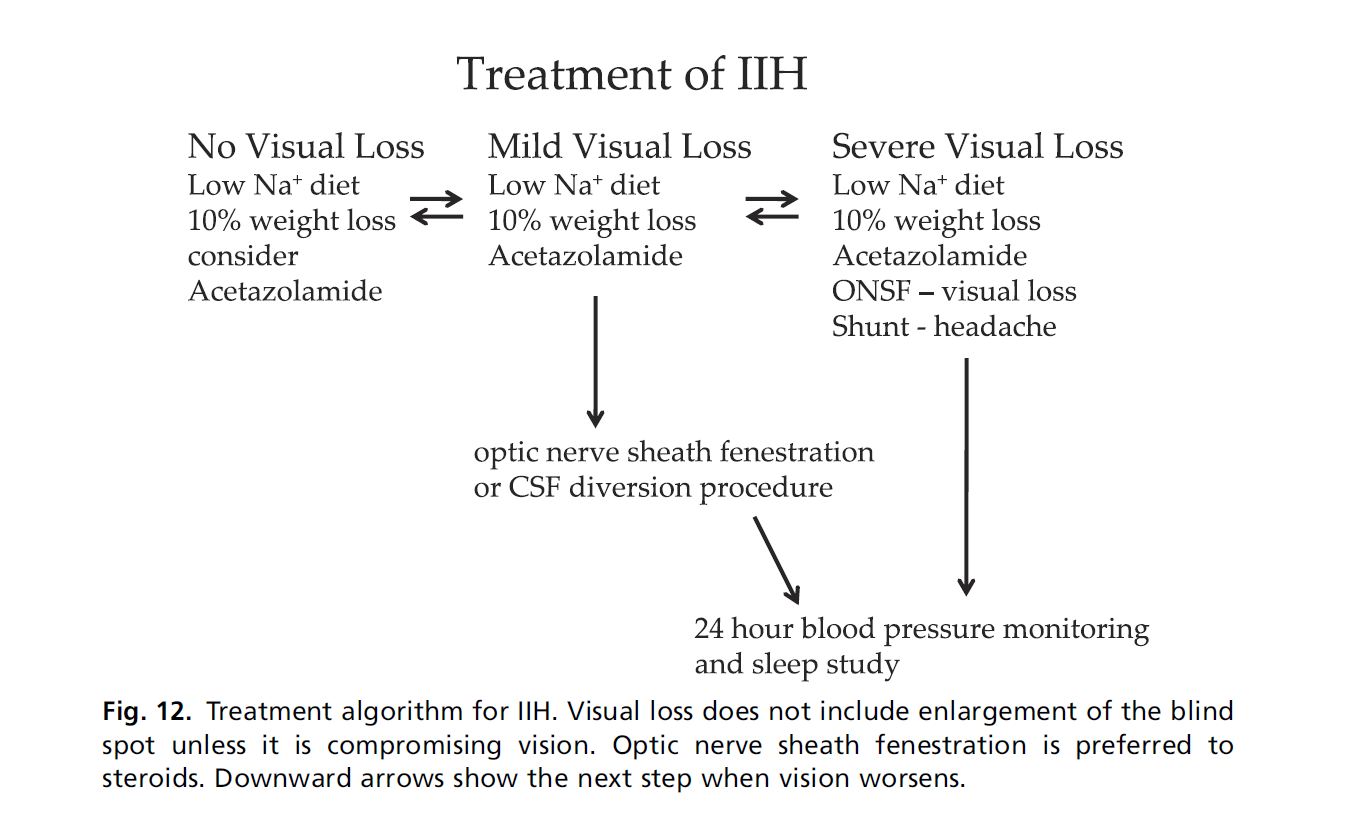
The second surgical procedure, called CSF shunting, is done as follows. Tubing is placed in the spinal fluid space, (either the space entered during a lumbar puncture or space in or around the brainand tubing is then run to the abdomen or a vein. This lowers the pressure around the brain and optic nerve, thereby eliminating the symptoms of raised intracranial pressure. Unfortunately, these procedures are complicated by various problems, the most severe one being some patients have periodic occlusion of the tubing with recurrence of symptoms and sometimes vision loss. A repeat operation is then needed. An overview of treatment is summarized in figure 12.
Management of the pregnant IIH patient
Pregnancy occurs in IIH as often as in the general population and in any trimester. Patients with IIH during pregnancy do not have an increased spontaneous abortion rate. Therapeutic abortion to limit progressive disease is not indicated. The pregnant patient with IIH should be treated as any other patient with IIH. Also, the pregnancy should be managed like any other. The major exception is caloric restriction because of its adverse effect of ketosis on the fetus. Weight gain can be limited to 20 pounds or the amount recommended by an obstretician.
Use of corticosteroids has not been associated with birth defects in humans. Acetazolamide may be used after 20 weeks gestation; use before 20 weeks has been associated with one case of sacrococcygeal teratoma. Glycerol and thiazide diuretics probably should not be used in the second half of pregnancy because of the risk of decrease in placental blood flow. There is no obstetric contraindication to surgery for those that require it.
Continue with How is IIH treated: The Idiopathic Intracranial Hypertension Treatment Trial
Return to IIH Index


