Keratoprosthesis
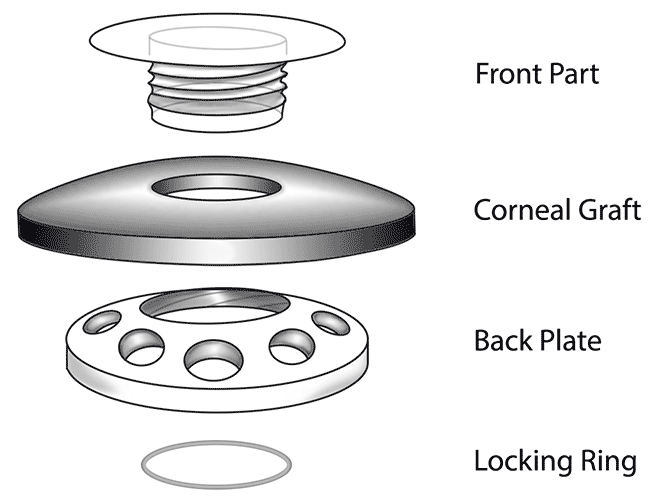
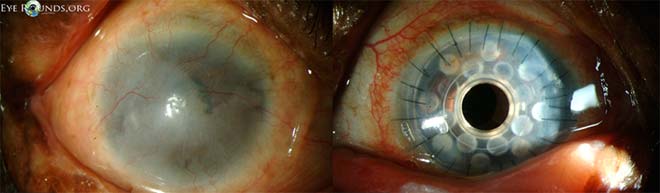
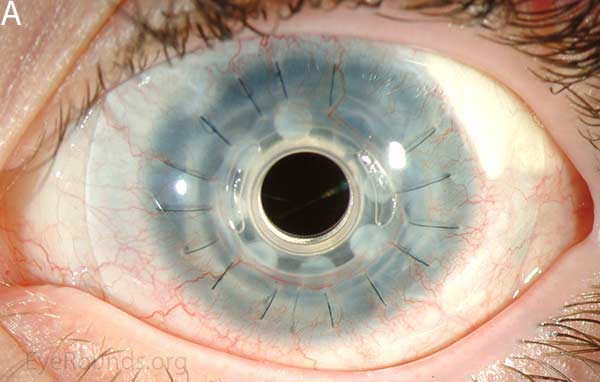
Keratoprosthesis implantation is a procedure that involves full-thickness removal of the cornea and replacement by an artificial cornea. The Boston Type I Keratoprosthesis is currently the most commonly used keratoprosthesis device in the US. It consists of a clear plastic polymethylmethacrylate (PMMA) optic and back plate sandwiched around a corneal graft and secured with a titanium locking ring (Figure 15). After the device is assembled, a partial-thickness trephination is performed on the host cornea. Full-thickness resection of the patient's cornea is then completed using curved corneal scissors. The keratoprosthesis is then secured to host tissue using interrupted or running sutures. Generally, patients who have a history of multiple failed PKs are candidates for a keratoprosthesis transplant. Other indications include severe keratitis or ocular surface disease resulting from limbal stem cell failure, such as Stevens-Johnson syndrome (Figure 16), ocular cicatricial pemphigoid, aniridia (Figure 17) and chemical injury (1, 13). The Boston Type II Keratoprosthesis is a similar device with a longer optic designed to extend through an opening made in the upper eyelid (Figure 19). It is indicated for the most severe cicatrizing ocular surface diseases.
 |
 |
 |
 |
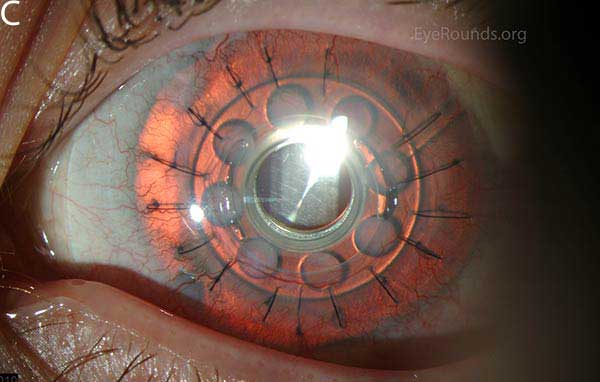 |
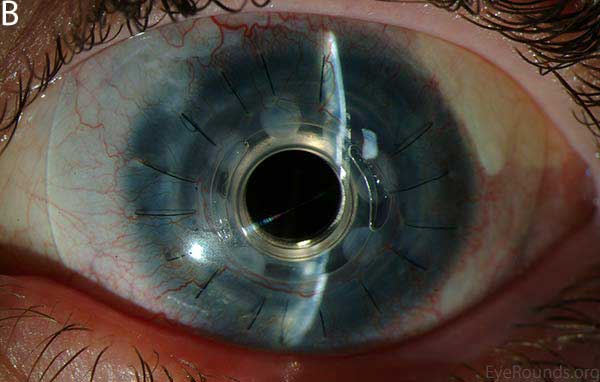
 A |
 B |
KPro placement offers relatively fast visual rehabilitation. The devices are amenable for use in many situations in which other types of keratoplasty are not an option.
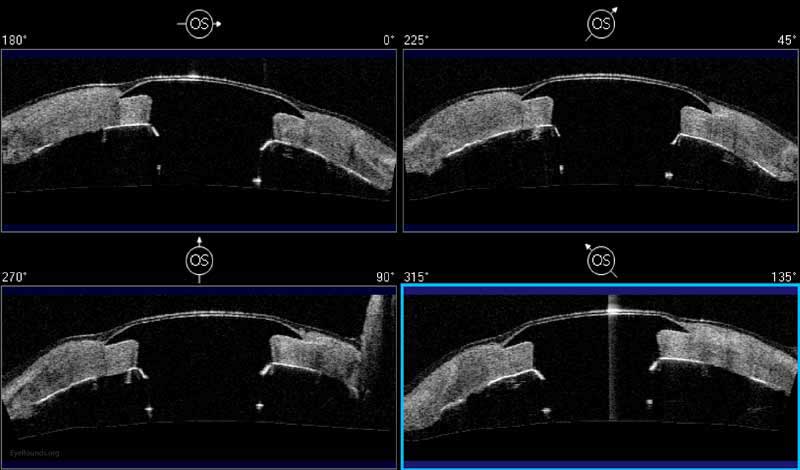
There is significant long-term risk of complications for those with a keratoprosthesis. Because the KPro is a foreign body, there is risk of infection or extrusion of the device. Post-operative glaucoma is common and intraocular pressure is difficult to evaluate as the hard optic makes traditional tonometry impossible. For this reason, glaucoma tube shunts are typically placed at the time of the corneal transplant at the University of Iowa. The Diaton is currently the preferred way to measure intraocular pressure in these patients in our institution. Patients can form retroprosthetic membranes requiring treatment with a Nd:YAG laser or surgical membranectomy (21).
Basic procedure steps (Video 5):
- Mark the center of the host cornea using a Sinskey hook and measure the cornea to determine the appropriate transplant size.
- Trephine the donor cornea.
- Assemble the keratoprosthesis by sandwiching the corneal graft between the front and back plates of the KPro device.
- Trephinate the host cornea to approximately 90% depth.
- Create a paracentesis, in the trephination groove or the corneal periphery, and inject Healon into the anterior chamber to preserve anterior chamber depth and stability.
- After using a blade to enter the eye through the trephination groove, resect the host cornea tissue using curved corneal scissors.
- Secure the donor tissue of the assembled KPro to the host corneal tissue using interrupted and/or running 9-0 nylon sutures.
- Rotate the sutures to bury the knots.
Additional Resources:
Video Links
Articles