Thyroid Eye Disease: An Introductory Tutorial and Overview of Disease
Workup and Diagnosis
Differential Diagnosis
When examining a patient with suspected TED, it is important to have a working differential. The following diagnoses share some similarities to the clinical presentation of TED
- Allergic conjunctivitis – While both can cause excess tearing and conjunctivitis, allergic conjunctivitis tends to be acute in onset from a new exposure, causes itching, can have papillary conjunctival reaction, and is not associated with eyelid retraction or exophthalmos (Figure 18).
Figure 18: Allergic conjunctivitis. Note the presence of giant papillae.(larger image not available)
- Myasthenia gravis (MG) – Like TED, MG patients can present with diplopia. However, MG tends to worsen throughout the day and improves after rest while diplopia in TED is not typically variable. Also, MG patients may present with ptosis, which is not associated with TED. Diplopia associated with TED is restrictive in nature, which can be determined by forced duction testing.
- Orbital myositis (OM) – OM causes enlargement and inflammation of the muscle body and tendon insertion, rather than just the muscle body, as is the case in TED patients. Orbital myositis is not generally associated with eyelid retraction. OM is usually unilateral. A bilateral presentation would be unusual for OM, whereas TED can present either way.
- Orbital tumors – Orbital tumors are typically unilateral in presentation and can cause proptosis and a wide variety of motility disturbances depending on location. Orbital tumors are unlikely to cause eyelid retraction or lid lag. (see Eye Rounds case on Cavernous Hemangioma)
- Carotid-cavernous fistula (CCF) – Patients may hear pulse-synchronous tinnitus. Presentation may include proptosis, pulsatile exophthalmos, dilated conjunctival and episcleral vessels, elevated intraocular pressure, or enlarged EOM depending on the amount of flow through the fistula and the degree of congestion. A CCF would not cause eyelid retraction or temporal flare. (see Eye Rounds case on CCF)
- Chronic progressive external ophthalmoplegia (CPEO) – CPEO slowly progresses over 5-15 years with most patients presenting with ptosis. All cardinal directions of gaze are affected, with downgaze most likely spared. TED, conversely, typically affects downward and nasal gaze.
- Inflammatory orbitopathy, such as granulomatosis with polyangitis (GPA, formerly known as Wegener's granulomatosis) – GPA typically presents with a mix of upper airway, lower airway, and renal pathologies. Patients may have conjunctivitis, episcleritis, scleritis, and/or uveitis. Other than conjunctivitis, these findings are uncommon in TED patients.
- IgG4 disease – Tumefactive lesions and fibrosis affecting one or more organs characterize this fibro-inflammatory disorder. It is most commonly present in the biliary tree, retroperitoneum, salivary glands, orbit, and lymph nodes. It is thought to involve both humoral and cell-mediated immunity. Orbital IgG4 disease often involves painless swelling of the extraocular muscles, lacrimal glands, and infraorbital nerves in combination with paranasal sinus disease. IgG4 disease can also present as an inflammatory orbital mass lesion.
Clinical Requirements for Diagnosis
In diagnosing TED, two of the following three clinical requirements must be met [13 ,14]
- Laboratory evidence (current or recently-treated immune-related thyroid dysfunction)
- Graves' disease
- Hashimoto's thyroiditis
- Presence of thyroid antibodies without a dysthyroid state: TRA, thyroid-binding inhibitory antibodies, TSI, antimicrosomal antibody
- Exam findings (1 or more of the following)
- Unilateral/bilateral eyelid retraction with temporal flare
- Unilateral/bilateral proptosis
- Restrictive strabismus
- Compressive optic neuropathy
- Fluctuating eyelid edema/erythema
- Chemosis/caruncular edema
- Radiographic evidence: unilateral/bilateral fusiform enlargement of inferior rectus, medial rectus, super rectus/levator complex, or lateral rectus
Disease Stratification
If TED is suspected, one must determine disease activity and severity in order to assess the urgency of treatment.
Disease Activity
In assessing the activity level of TED in a patient, the clinical activity score (CAS) can be used [15].
- At the initial visit, patients are given a CAS score of 1-7, one point for each sign or symptom (Figure 19):
- Spontaneous orbital pain in the last 4 weeks
- Gaze evoked orbital pain in the last 4 weeks
- Eyelid swelling that is considered to be due to active TED
- Eyelid erythema
- Conjunctival injection considered to be due to active TED
- Chemosis
- Inflammation of caruncle or plica semilunaris
- At follow-up visits, add the 3 following criteria for a potential CAS score of 10 (one point for each sign or symptom)
- Increase of ≥ 2 mm in proptosis
- Decrease in uniocular motility in any one direction of ≥ 8 degrees
- Decrease in visual acuity equivalent to 1 Snellen line
- TED is considered "active" if the CAS ≥ 3 at the initial visit or ≥ 4 at follow-up visits [16].
|
|
Disease Severity
In classifying the severity of TED, 3 indices are typically used
- The Werner's NOSPECS measures clinical severity based on presenting features [17]
- Class 0: No signs or symptoms
- Class 1: Only signs (upper lid retraction and stare, ± lid lag)
- Class 2: Soft tissue involvement (edema of conjunctiva and lids, conjunctival injection)
- Class 3: Proptosis
- Class 4: Extraocular muscle involvement (usually with diplopia)
- Class 5: Corneal involvement (primarily lagophthalmos)
- Class 6: Sight loss (due to optic nerve involvement)
- The European Group Of Graves' Orbitopathy (EUGOGO) reports that TED severity can be classified by the following measurements [16]
- Assess for an RAPD
- Record lid retraction (Figure 20)
- MRD 1 (note superior scleral show)
- MRD 2 (note inferior scleral show)
- Note if temporal flare is present
- Hertel exophthalmometer with intercanthal distance
- Risk of cornea ulceration
- Lagophthalmos
- Bell's Phenomenon (if absent, eye will not rotate up and out with lid closure)
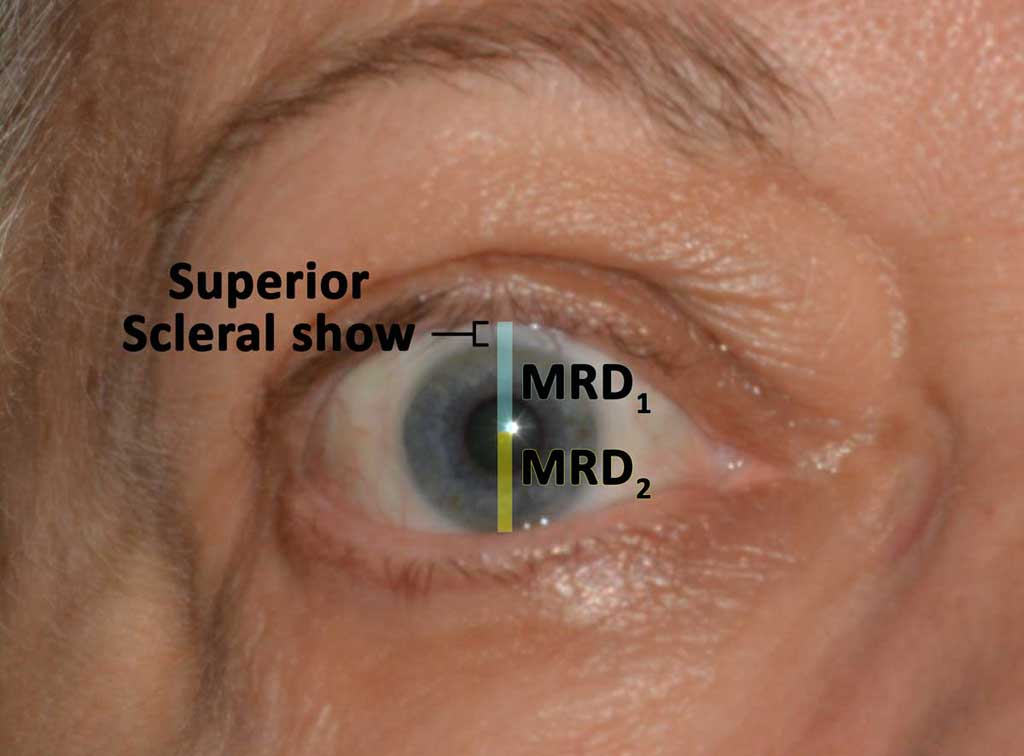
Figure 20: External eye measurements. This patient has lid retraction and superior scleral show. A demonstration of the MRD1 and MRD2 calculations is shown here.
- EUGOGO has also proposed a classification scheme that grades TED as mild, moderate-to-severe, and sight-threatening based on the following criteria [16]
- Mild
- Mild impact on daily life
- Insufficient to justify immunosuppressive/surgical treatment
- One or more of the following
- Minor lid retraction (< 2 mm)
- Mild soft tissue involvement
- Exophthalmos < 3 mm above normal for race and gender (~18 mm for Asians, 20 mm for Caucasians, and 22 mm for African Americans)
- Transient or no diplopia
- Corneal exposure responsive to lubricants
- Moderate-to-severe
- Non-sight-threatening but sufficient impact on life to justify immunosuppression or surgical intervention
- One or more of the following
- Lid retraction ≥ 2 mm
- Moderate or severe soft tissue involvement
- Exophthalmos ≥ 3mm above normal for race and gender
- Transient or constant diplopia
- Sight-threatening
- TED patients with resultant optic neuropathy and/or corneal breakdown
- Warrants immediate intervention
- The VISA analysis (Vision, Inflammation, Strabismus, and Appearance) subjectively and objectively evaluates each category, which is based on the presence and severity of signs and symptoms (Figure 21).
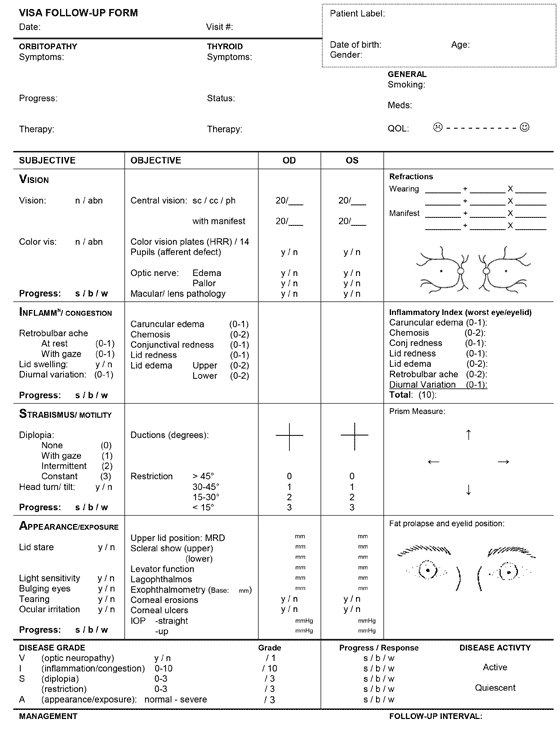 (click image for pdf)
(click image for pdf)
Figure 21: VISA chart


